Myeloma Chinese: Expert Interpretation of Guidelines for Response Assessment and Diagnostic System in Multiple Myeloma
Myeloma Chinese: Expert Interpretation of Guidelines for Response Assessment and Diagnostic System in Multiple Myeloma
Multiple myeloma is a malignant tumor originating from bone marrow stromal cells. In recent years, with the application of new treatment methods, the early mortality rate of multiple myeloma patients has been significantly reduced, and the prognosis of multiple myeloma patients has been improved. Early identification of multiple myeloma and precise risk stratification are crucial for treatment. Whole-body magnetic resonance imaging (WB-MRI) is currently the most sensitive technique for bone marrow imaging, which can detect bone marrow infiltration early and has been increasingly used in the diagnosis and treatment of multiple myeloma in recent years. However, the WB-MRI technique is complex, and it is necessary to establish standardized image acquisition and reporting standards to promote its wider application.
In 2019, an international, multidisciplinary expert panel composed of radiologists, medical physicists, and hematologists with experience in WB-MRI diagnosis of multiple myeloma, referring to the Prostate Cancer Metastasis Reporting and Data System, formulated the Myeloma Response Assessment and Diagnosis System (MY-RADS) and published it in Radiology. The aim was to promote standardization and reduce differences in the acquisition, interpretation, and reporting of WB-MRI images for multiple myeloma. Although MY-RADS has been published for some time, its clinical application is still insufficient. This article will interpret MY-RADS to better popularize and promote it.
I. Advantages and Limitations of WB-MRI
X-ray and CT primarily detect the destruction of trabecular bone and cortical bone caused by multiple myeloma, but have limited sensitivity for bone marrow infiltration that has not yet caused bone destruction. WB-MRI can directly image the bone marrow with high sensitivity. PET-CT can also be used to diagnose focal bone lesions, but its sensitivity is lower than that of DWI. DWI not only has high sensitivity but can also quantitatively evaluate treatment response and heterogeneity before changes in lesion size using the ADC value. However, the specificity of DWI is still controversial, and it is not feasible to biopsy all lesions. The International Myeloma Working Group recommends follow-up of 3-6 months for isolated small equivocal lesions.
II. MY-RADS WB-MRI Data Acquisition Standards
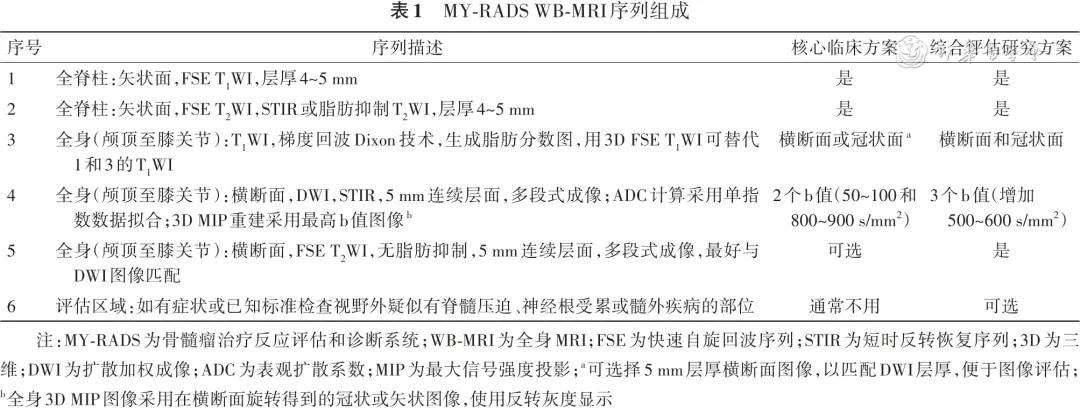
MY-RADS provides two data acquisition schemes: a core clinical protocol for disease detection and diagnosis, recommended to be completed within 30 minutes, and a comprehensive assessment research protocol for evaluating soft tissue or extramedullary infiltration, recommended to be completed within 45-50 minutes. Scanning can be performed on 1.5T or 3.0T scanners, and it is recommended that the baseline and follow-up images of the patient be acquired on the same machine. The sequence composition of the two schemes is shown in Table 1.
III. Collection of Clinical Information
Ideally, radiologists should obtain the following information (which can be queried from electronic medical records) when reporting: the time of initial diagnosis or suspected diagnosis, serum M-protein and light chain levels, bone marrow cytology and bone marrow aspiration site (if performed), presence of clinical symptoms or signs of spinal cord or nerve root compression and the specific location, whether it is the initial examination or follow-up, current treatment situation, history of autologous or allogeneic stem cell transplantation, details of previous radiation therapy or surgical intervention (including vertebroplasty, granulocyte colony-stimulating factor or steroid use, minimal residual disease), etc.
IV. WB-MRI Imaging Evaluation
Image evaluation should use image linking, workstation facilities, and co-registration tools as diagnostic aids, combining all DWI images (low, intermediate, and high b-value images and ADC maps) with anatomical and fat fraction images for multisequence evaluation. The evaluation of low signal and high signal on high b-value (800-900 s/mm2) DWI images is subjective and can use adjacent muscle as a reference, while the evaluation of ADC maps should use quantitative data.
Factors such as bone marrow edema caused by osteoarthritis, infection, fracture, liquefaction after effective treatment of focal lesions, osteonecrosis, vertebral hemangioma, chondroma, cyst, focal bone marrow fat deficiency, and artifacts around metal implants can all present as high signals on high b-value DWI images, causing false positives. Therefore, it is necessary to perform a comprehensive evaluation based on morphological features (T1WI and Dixon images) and ADC values (normal bone marrow ADC values are usually below 0.7×10-3 mm2/s, while active tumor tissues range from 0.7×10-3 to 1.4×10-3 mm2/s). Since ADC values are affected by many factors, the evaluation of tumor infiltration cannot rely solely on the recommended ADC cutoff values.
1. Lesion Size Measurement: The International Myeloma Working Group defines a threshold of 5 mm for a definite focal active lesion, and lesions >5 mm should be recorded as focal active lesions. However, due to the limitations of image resolution, size changes should be measured on lesions ≥10 mm. In individual cases where all lesions are <10 mm, size measurement can be performed if the lesions are confirmed as malignant and the image resolution is known.
2. ADC Measurement: ADC measurement should be combined with DWI images, and the measurement region should ideally show high signal on all b-value DWI images or at least on low and intermediate b-value images. ADC is generally considered a reproducible parameter, with a low coefficient of variation of 2.8% in myeloma-involved bone marrow.
3. Evaluation of Diffuse Bone Marrow Infiltration: For newly diagnosed or suspected multiple myeloma patients, diffuse signal reduction on fast spin-echo T1WI or in-phase and fat images of the Dixon sequence, and diffuse signal increase relative to normal muscle on high b-value DWI images, may suggest diffuse bone marrow infiltration. However, diffuse bone marrow infiltration must be confirmed by biopsy, and imaging examination is necessary to ensure the biopsy site is representative (i.e., hitting the diffusely involved bone marrow). ADC measurement of diffuse bone marrow infiltration should be performed in the area of diffuse marrow infiltration, with an ROI area >1 cm2.
In untreated and newly diagnosed multiple myeloma patients, a bone marrow ADC >0.7×10-3 mm2/s can increase the diagnostic confidence of diffuse bone marrow infiltration. For treated patients, the possibility of false positives for diffuse bone marrow infiltration increases due to reactive cell proliferation associated with granulocyte colony-stimulating factors. Therefore, the use of granulocyte colony-stimulating factors must be ruled out when suspecting diffuse bone marrow infiltration. If disease progression is suspected solely due to suspicion of diffuse bone marrow infiltration, it must be confirmed by serum biochemistry and/or bone marrow biopsy.
V. Treatment Response Assessment (Response Assessment Categories, RAC)
The guidelines recommend a structured clinical report for each examination. If the patient is undergoing a follow-up examination, the results of multiple examinations should be compared to assess the response to treatment. The guidelines divide the body into seven anatomical regions: cervical spine, thoracic spine, lumbar spine, pelvis, long bones, skull, and ribs/others. The RAC is classified into five categories: 1, highly likely response; 2, likely response; 3, stable disease; 4, likely progression; 5, highly likely progression.
1. Highly Likely Response:
(1) Previously involved areas with focal or diffuse marrow infiltration return to normal fatty marrow;
(2) Significant decrease in the number or size of focal lesions;
(3) Diffuse marrow infiltration converts to scattered nodules, with a significant decrease in tumor burden within the corresponding marrow cavity;
(4) Decrease in soft tissue changes associated with bone lesions;
(5) Appearance of intra-lesional or peri-lesional fat (fat dots or halo sign) within or around focal lesions;
(6) ADC increase in previously representative lesions (representative lesions: the guidelines recommend selecting ≤5 lesions per region for measurement of lesion size and ADC, and these selected lesions are considered representative lesions, typically larger lesions with significantly increased DWI signal, easily identifiable by the naked eye, and convenient for measurement) from ≤1.4×10^-3 mm^2/s to >1.4×10^-3 mm^2/s;
(7) Lesion ADC increases ≥40% compared to baseline, with corresponding signal decrease on high b-value DWI images, and morphological findings consistent with stable or responsive lesions;
(8) Changes in soft tissue lesions meet the criteria for complete response or partial response according to the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1.
2. Likely Response: Evidence of improvement, but not sufficient to meet the criteria for RAC 1.
(1) Slight decrease in the number or size of focal lesions;
(2) ADC increase in previously representative lesions from ≤1.0×10^-3 mm^2/s to >1.4×10^-3 mm^2/s;
(3) Lesion ADC increases >25% but <40% compared to baseline, with corresponding signal decrease on high b-value DWI images, and morphological findings consistent with stable or responsive lesions;
(4) Soft tissue lesion changes do not meet the criteria for partial response according to RECIST v1.1.
3. Stable Disease: No significant change observed.
4. Likely Progression:
(1) Evidence of worsening lesions, but not sufficient to meet the criteria for RAC 5;
(2) Equivocal appearance of new lesions;
(3) No change in lesion size, but increased signal intensity on high b-value DWI images (ADC <1.4×10^-3 mm^2/s), consistent with possible disease progression;
(4) Recurrent lesions, defined as the reappearance of previously resolved lesions or enlargement of previously partially responding or stable lesions after treatment;
(5) Intraspinal soft tissue lesions causing spinal canal stenosis, but unrelated to neurological symptoms and not requiring radiation therapy;
(6) Soft tissue lesion changes do not meet the criteria for disease progression according to RECIST v1.1.
5. Highly Likely Progression:
(1) New pathological fractures or spinal cord compression requiring radiation therapy or surgical intervention, confirmed as malignant lesions by MRI signal characteristics;
(2) Definite new lesions with a diameter >5 mm or diffuse marrow infiltration in previously normal marrow areas;
(3) Significant increase in the number or size of focal lesions;
(4) Focal lesions evolving into a diffuse infiltration pattern;
(5) Appearance or increase of soft tissue lesions associated with bone lesions;
(6) Appearance of new high-signal lesions or areas on high b-value DWI images, with ADC of 0.6×10^-3 to 1.0×10^-3 mm^2/s;
(7) Soft tissue lesion changes meeting the criteria for disease progression according to RECIST v1.1.
VI. Structured Reporting
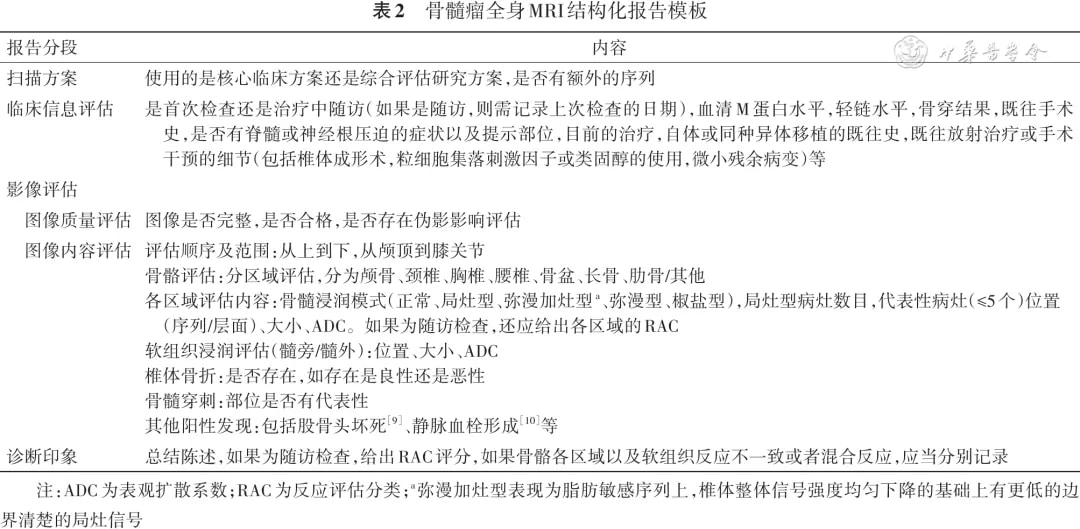
Structured reporting can improve report quality, reduce variability among physicians, and facilitate data mining for research. Based on the MY-RADS template and the practical experience of the team, a structured clinical report template has been developed, including scanning protocol, clinical information assessment, image assessment (image quality assessment and image content assessment), and diagnostic impression (Table 2).
VII. Clinical Trial Assessment
Most clinical reports can follow the structured reporting format outlined above. However, medical centers aiming to collect cases for clinical trial evaluation may require a more complex scoring system. For this purpose, the guidelines propose a comprehensive MY-RADS scoring system for advanced or clinical trial evaluations.
The scoring system is applied sequentially for each anatomical region: cervical spine, thoracic spine, lumbar spine, pelvis, long bones, skull, and ribs/others. For each anatomical region, the number of lesions, the size of the largest lesion, the location, size, ADC, and signal intensity changes (for follow-up) of the target lesions should be recorded, as well as the RAC (for follow-up). Finally, the overall tumor burden score and the overall RAC should be provided.
The evaluation should consider the following:
(1) The size of bone marrow lesions should be measured on T1-weighted images, and signal changes should be assessed on DWI;
(2) If diffuse infiltration is suspected, the number of lesions should be marked as “diffuse.” If diffuse infiltration is confirmed, the D score is D1; if unconfirmed, the D score is Dx;
(3) For focal infiltration, the number of active lesions should be indicated. If there are ≥10 lesions, the score is 3; if there are 2-9 lesions, the score is 2; if there is 1 lesion, the score is 1; if there are no lesions, the score is 0. The diameter of the largest lesion should also be recorded. If the diameter is >15 mm, the score is 3; if it is 5-15 mm, the score is 2; if it is <5 mm, the score is 1;
(4) The overall tumor burden (D score) is considered high if there are ≥10 focal lesions, or ≥1 lesion located within an axial bone (vertebral body or pelvic bone) and ≥10 mm in diameter.
The overall tumor burden score includes the D score (diffuse), F score (focal), and E score (extramedullary). For example, if a patient has confirmed diffuse signal involvement in 6 anatomical regions by bone marrow aspiration, the D score is D6. If the diffuse infiltration signal is not confirmed by bone marrow aspiration, the D score is D6x. If the same patient also has focal lesions, with 1 lesion in the thoracic spine (score 1), and the lesion is >15 mm (score 3); and 4 lesions in the pelvis (score 2), with lesions <5 mm (score 1), the total score would be D6F7. If the patient also has extramedullary lesions, the score is D6F7E+; if there are no extramedullary lesions, the score is D6F7E-. Extramedullary/extraosseous lesions should be evaluated for treatment response according to RECIST v1.1, with a maximum of 5 lesions recorded, including location, slice, and size, and the overall follow-up RECIST v1.1 status documented. If this is a follow-up examination, the overall imaging impression should be considered, and the primary RAC should be recorded. If another response pattern is observed, a secondary RAC can be recorded. The primary RAC is the response pattern observed in most lesions within a region, while the secondary RAC records the second most common response pattern within the region.
VIII. Summary and Outlook
MY-RADS is a comprehensive guideline that provides reference standards for the acquisition, interpretation, and reporting of whole-body MRI (WB-MRI) for bone marrow lesions. The proposed Response Assessment Categories (RAC) for bone marrow lesions provide an MRI imaging standard for evaluating treatment response in patients with bone marrow lesions, which is an innovation compared to traditional response criteria and minimal residual disease response criteria. MY-RADS proposes a structured reporting template for bone marrow lesion WB-MRI, as well as a comprehensive MY-RADS scoring system for advanced or clinical trial evaluations, which have significant application value in quantifying lesions and promoting research standardization. The structured reporting is relatively complex, but it is recommended for adoption. The workload for physicians can be reduced by stating that “this examination is focused on the bone marrow and is not a comprehensive examination of the brain, lungs, abdominal organs, etc.,” thereby minimizing the need for descriptions of other organs.
Research has demonstrated the good applicability of the MY-RADS guidelines in evaluating treatment response in multiple myeloma. The RAC criteria can independently stratify patients and better predict prognosis. The combined use of RAC and multiparametric flow cytometry can more precisely evaluate minimal residual disease. Additionally, MY-RADS can be used for multicenter studies, enabling all centers to obtain high-quality images suitable for qualitative and quantitative analysis. Furthermore, research has shown that low RAC scores can predict deep responses in multiple myeloma, but this is only applicable to non-anemic patients, as anemic patients often exhibit conversion of spinal marrow to red marrow, which can affect the assessment of marrow infiltration in multiple myeloma.
The application of MY-RADS is still limited, and future research is needed to evaluate its role in predicting prognosis in patients with bone marrow lesions and its correlation with other response assessment criteria. Moreover, future studies can leverage artificial intelligence to enhance MY-RADS, making diagnostic and treatment response assessments more convenient. The WB-MRI techniques and the recommended structured reporting template involved in MY-RADS are relatively complex, requiring promotion and dissemination to increase their adoption rate and consistency of application in China.
Content Source:中华放射学杂志
