Successful Cases of CAR-T Diffusion Large B Cell Lymphoma in the Treatment of Advanced Patients
Successful Cases of CAR-T Diffusion Large B Cell Lymphoma in the Treatment of Advanced Patients
“CR Dawn” is a column launched by Lymphoma Home, aimed at sharing the recovery stories of lymphoma patients and showcasing the miracles of life and medicine. This column focuses on patients and doctors who have experienced tortuous treatments but eventually welcomed the dawn, presenting their tenacity and courage in fighting against lymphoma through in-depth interviews. Through the explanations of doctors, fellow patients can gain a deeper understanding of treatment plans and new drugs, providing references for their own treatment decisions. As long as they maintain confidence and actively cooperate with the treatment, the dawn of life will surely appear.
In this issue of the “CR Dawn” column, Lymphoma Home interviewed Professor Yang Jianmin, the director of the Department of Hematology at Changhai Hospital. In May 2023, he successfully saved a young patient with critical relapsed/refractory primary central nervous system lymphoma (PCNSL) through autologous stem cell transplantation (ASCT) sequential CAR-T cell therapy.
Case Details
Patient: Male, 29 years old.
Disease Onset and Treatment History
December 2018: Onset with headache.
December 18, 2018: Examination results as follows:
PET-CT: A high metabolic density lesion (about 3.4*1.9 cm, SUVmax=34.4) was seen in the left frontal lobe and genu of the corpus callosum, with significantly increased FDG metabolism.
Biopsy pathology and immunohistochemistry: Diffuse large B-cell lymphoma (NOS, GCB).
Immunophenotype: Ki67(50%+), CD19(+), CD20(+), PAX5(+), CD79(+), MUM1(+), BCL(+), CD10(-/+), CD2(few+).
Cerebrospinal fluid examination: 6% morphologically abnormal immature lymphoid cells.
Diagnosis: Primary central nervous system lymphoma (DLBCL, GCB)
Treatment at another hospital:
Treatment at our hospital:
May 9, 2023: Autologous stem cell reinfusion.
May 24, 2023: Autologous CD19 CAR-T cell reinfusion.
August 30, 2023: Evaluation showed complete remission (CR), and the patient has now returned to normal life.

Interview with the Attending Physician
For relapsed/refractory (R/R) PCNSL, on the pathological level, the tumor cells are highly malignant and progress rapidly; on the patient level, the involvement of the brain is significant, leading to poorer function of other organs, and neurological function and physical condition often deteriorate rapidly. Therefore, rapid diagnosis, timely treatment, and selecting the appropriate treatment plan are crucial. This patient was young, and the previous treatment at another hospital involved multiple courses of high-dose chemotherapy, but the desired effect was never achieved. How to quickly reverse the critical condition and achieve CR was an important challenge for the patient upon admission to our hospital.
ASCT + CAR-T was the best treatment plan we considered comprehensively. ASCT was performed first to play a pretreatment role, reducing the tumor burden while improving the suppressive effect of the lymphoma immune microenvironment on CAR-T cells. Subsequently, CAR-T therapy was bridged to achieve specific killing of tumor cells through the modification of the patient’s T cells, further eradicating residual lesions after ASCT and reducing the risk of tumor recurrence.
This case demonstrated the near “life-saving” potential of the ASCT + CAR-T treatment regimen, with the patient regaining consciousness within a month of entering the transplant ward. In actual clinical practice, we observed that using ASCT + CAR-T to treat lymphoma can achieve a CR rate of 70-80%, realizing a synergistic effect of 1+1>2, offering hope for a cure.
Suggestions for PCNSL Patients from This Case
Primary central nervous system lymphoma (PCNSL) is a rare extranodal subtype of non-Hodgkin’s lymphoma, with over 95% of patients having the pathological type of diffuse large B-cell lymphoma. PCNSL has the worst prognosis among all non-Hodgkin’s lymphomas, with a median overall survival of 1.3 years according to statistics.1 For many patients and their families, the treatment and management of PCNSL remain a challenging and unknown path.
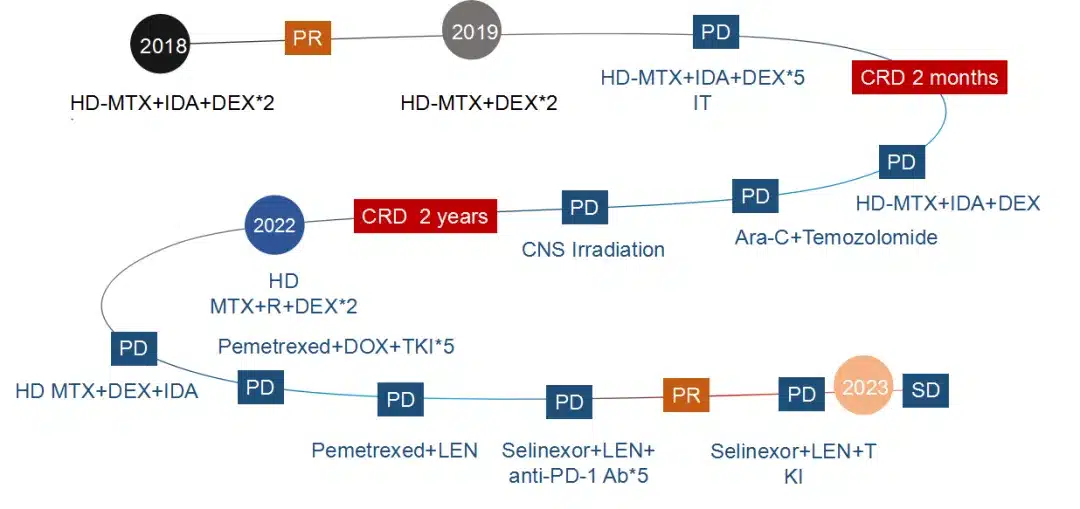
In this case, the patient received a combined chemotherapy regimen based on high-dose methotrexate (HD-MTX) as first-line treatment, achieving only a partial remission (PR), and progressed within a year (PD). Subsequently, the patient underwent various salvage chemotherapy regimens, radiation therapy, and combination with targeted drugs such as the XPO1 inhibitor, but the effect remained poor. Upon admission, the patient was drowsy and could only be awakened occasionally, unable to take care of themselves, and experiencing persistent seizures. After attempting various treatment regimens, the choice of the next treatment and how to achieve further remission became not only a treatment challenge for this patient but also a therapeutic bottleneck faced by most patients with relapsed/refractory (R/R) PCNSL.
ASCT plays an important role in the consolidation treatment of PCNSL, but the benefits it can bring are limited. Real-world research has found that only 17% of R/R PCNSL patients can benefit from ASCT.2 With the advent and continuous progress of CAR-T therapy, it has demonstrated tremendous potential in the field of hematological malignancies, including lymphoma, and its application in DLBCL and R/R PCNSL has also been validated by numerous studies. Therefore, using CAR-T for consolidation treatment after ASCT may effectively improve the survival rate and quality of life for PCNSL patients.
ASCT + CAR-T: A Powerful Combination Bringing Survival Benefit to PCNSL Patients
ASCT first eliminates residual tumor cells in the body through pretreatment measures such as high-dose chemotherapy, and then rebuilds the immune system using the patient’s own hematopoietic stem cells. To a certain extent, this method can prolong the patient’s survival. However, the patient may not receive the desired benefit due to complications or ineffective salvage treatment.
CAR-T is currently the only novel treatment modality with evidence of long-term survival and the potential for cure. By modifying the patient’s own T cells, it enables them to recognize and kill tumor cells. Currently, the largest cohort study on CAR-T treatment for PCNSL has confirmed that anti-CD19 CAR-T therapy is effective for heavily pretreated R/R PCNSL patients, with a high remission rate and a CR rate of up to 86%. In the third-line or later treatment setting, 46% of R/R PCNSL patients achieved long-term remission, better than previously observed outcomes. Moreover, the safety of anti-CD19 CAR-T treatment for patients is controllable.2
Therefore, ASCT sequential CAR-T can effectively improve the survival of R/R PCNSL patients, providing a new treatment option and hope for a cure for PCNSL patients.
Aim for Cure: Earlier CAR-T Treatment Brings More Benefits
In recent years, CAR-T therapy has made tremendous progress in the field of lymphoid and hematological malignancies, significantly changing the clinical treatment paradigm. For patients with rapidly progressing, poor prognosis, and easily relapsing conditions after existing treatment regimens, such as PCNSL, early diagnosis, timely treatment, and achieving deep remission to the greatest extent possible in the front-line or even first-line setting is crucial. Early application of CAR-T therapy not only reduces tumor cell proliferation and spread but also lowers the risk of recurrence. A series of studies on Axi-cel in large B-cell lymphoma, including ZUMA-1 (3rd line or later), ZUMA-7 (2nd line), and ZUMA-12 (high-risk 1st line), have confirmed that as the treatment line moves forward, the survival benefit brought by Axi-cel continues to increase. Thus, earlier use of CAR-T can provide more clinical benefits for lymphoma patients and maximize their chances of achieving a cure.
Expert’s Message
In recent years, CAR-T therapy has gradually emerged as a promising treatment for lymphomas such as relapsed/refractory primary central nervous system lymphoma (R/R PCNSL). The exploration of combination treatment regimens centered on CAR-T is becoming increasingly popular. It is anticipated that the indications and accessibility of CAR-T can continue to expand, facilitating the realization of precision treatment and refined disease management for lymphomas, bringing new hope to patients with lymphomas and other hematological malignancies. As physicians, we sincerely hope that more lymphoma patients can achieve deeper remission, improved survival benefits, regain health, and enjoy the beauty of life with the help of novel therapies such as CAR-T. We hope that every patient can bravely move forward on the path of treatment and embrace their own dawn of cure.
References
1.中华医学会血液学分会淋巴细胞疾病学组,等. 白血病·淋巴瘤,2024,33(03):129-137.
2.Choquet S, et al. Am J Hematol. 2024 Apr 8.
Content Source:淋巴瘤之家086
