2024 EHA China Style Professor Pan Jing: Latest Progress of CART T Cell Lymphoma
2024 EHA China Style Professor Pan Jing: Latest Progress of CART T Cell Lymphoma
CAR-T cell therapy is flourishing in the field of hematological malignancies, including significant progress in the treatment of T-cell lymphomas. However, challenges such as relapse, off-tumor targeting, and viral infections urgently need to be addressed to further optimize the efficacy of CAR-T cell therapy. At the recent 2024 European Hematology Association (EHA) Annual Meeting, the research achievements of Professor Pan Jing’s team from Beijing Gaobeidian Hospital attracted widespread attention. Two studies focused on addressing the above issues and were both selected for oral presentations. Tumor Watch – Blood Newsletter invited Professor Pan Jing for an on-site interview to share and interpret the content of these two studies, aiming to provide valuable guidance and practical advice for CAR-T treatment of clinical T-cell lymphomas.
Abstract No.: S339
Previous-transplant or New-match Donor CD5 CAR-T Cells in Pediatric and Adult Relapsed/Refractory T-ALL: First-in-Human, Phase 1 Study
Study Introduction
Background
Relapsed/refractory acute T-cell lymphoblastic leukemia (r/r T-ALL) lacks effective salvage therapy and has a poor prognosis. Recently, CD7-targeted CAR-T cell therapy has shown efficacy in r/r T-ALL, but CD7-negative relapse is common. As CD5 is expressed in over 80% of T-ALL cells at diagnosis, it can serve as an alternative target for patients relapsing after or with low CD7 expression after CD7 CAR-T therapy.
Objective
This study aimed to evaluate the use of donor-derived CD5 gene-edited CD5 CAR-T cells in r/r T-ALL.
Methods
This single-center phase 1 study (NCT05032599) enrolled CD5+ r/r T-ALL patients to receive CD5 CAR-T cells (with CD5 gene knocked out by CRISPR-Cas9) derived from previous hematopoietic stem cell transplant (HSCT) donors (Cohort A) or new matched donors (Cohort B) (Dai et al. Mol Ther 2021;29:2707-2722). A Bayesian optimal interval (BOIN12) design was used to explore the optimal biological dose (OBD) with two target dose levels of 1–2×10^6/kg in both cohorts. If the manufactured CD5 CAR-T cell doses were suboptimal, patients received a lower dose of 0.5×10^6 (±20%)/kg. The primary endpoint was safety, and secondary endpoints included efficacy. Patients achieving complete remission (CR) after CD5 CAR-T infusion were recommended to receive HSCT consolidation. All patients or guardians provided written informed consent before screening.
Results
Between October 8, 2021, and March 21, 2023, 19 patients were enrolled, and 16 received CD5 CAR-T infusion, including 11 in Cohort A (7 at target dose) and 5 in Cohort B (3 at target dose). Ten (63%) patients relapsed from prior CD7 CAR-T therapy, with 5 having detectable CD7 CAR-T cells.
Adverse events (AEs) within 30 days included grade 3–4 cytopenias (100%, 92% pre-existing), grade 1–2 cytokine release syndrome (75%), grade 1–2 neurotoxicity (25%), grade 1 skin graft-versus-host disease (GVHD) (69%), and one grade 3 infection (6%). No dose-limiting toxicities (DLTs) occurred.
The CR with incomplete hematologic recovery (CRi) rate at day 30 post-infusion was 100% (16/16). As of July 31, 2023, with a median follow-up of 14.3 months (IQR, 6.2–19.7), 4 patients underwent HSCT at a median of 35 days (IQR, 31–40) post-infusion, with 3 remaining alive and disease-free and 1 dying from fungal infection; of the 12 non-transplanted patients (7 declined, 3 relapsed pre-HSCT, and 2 died during conditioning), 2 remained in remission, 3 relapsed, 5 died from infections (2 EBV and 3 bacterial), and 2 died from thrombotic microangiopathy. Half of the grade 5 infections occurred in patients with co-existing CD7 CAR-T cells who did not receive HSCT consolidation. Low-level CD7 CAR-T cells did not impact CD5 CAR-T expansion, with CD5 CAR-T cells remaining predominant until the last follow-up. CD5+ lymphocytes decreased, but CD5- lymphocytes increased, partially from CD5 gene-editing byproducts.
Conclusion
CD5 CAR-T cell therapy effectively induced CR in r/r T-ALL patients. However, the durability of remission was limited for non-transplanted patients who experienced increased risks of late severe infections, particularly those previously treated with CD7 CAR-T. Combining CD5 CAR-T therapy with HSCT consolidation may be a feasible approach to improve outcomes.
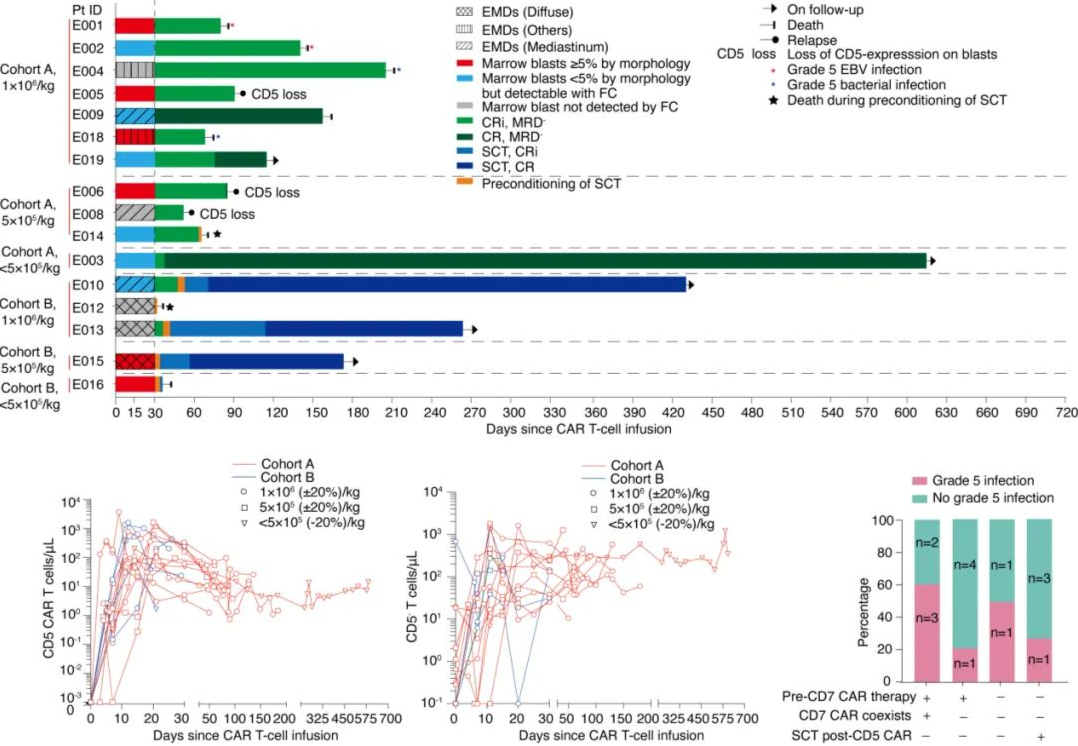
Image 1. Efficacy, expansion, and safety of CAR-T cells
Expert Interview
Tumor Watch – Blood Newsletter: At this year’s EHA meeting, you had two studies selected for oral presentations, which is a remarkable achievement. First, please introduce the background and main results of this study on previous-transplant or new-match donor CD5 CAR-T cell therapy for pediatric and adult relapsed/refractory acute T-cell lymphoblastic leukemia (r/r T-ALL).
Prof. Pan Jing: This clinical trial on CD5 CAR-T treatment for relapsed/refractory T-ALL began in 2019. During our research on CD7 CAR-T, we found that some patients experienced CD7-negative relapse after treatment, particularly around six months. This off-tumor target relapse after targeted therapy is common in all CAR-T treatments. To address this issue, we collaborated with Lundex Company, as they were conducting preclinical studies on CD5 CAR-T at that time and had published relevant articles, providing us with new insights. Therefore, we leveraged their preclinical data and translated it into the clinical process, successfully obtaining approval for the CD5 CAR-T clinical study.
From 2019 until now, this study has been ongoing for several years. As of now, the entire clinical trial has been completed. At this EHA meeting, we presented the overall data. In this study, we enrolled a total of 19 patients, of whom 16 successfully completed the CAR-T product infusion process. Notably, during the initial one-month treatment period, patients faced relatively low risks, with an overall response rate of 100%, as almost all patients achieved remission through CAR-T therapy. These enrolled patients were mainly those who experienced negative relapse after receiving CD7 CAR-T treatment. Therefore, CD5 CAR-T therapy was regarded as a salvage strategy for patients who failed CD7 CAR-T treatment. We established this project based on this research background.
Tumor Watch – Blood Newsletter: Based on the results of this study, what are your perspectives on combining CD5 CAR-T cell therapy with hematopoietic stem cell transplantation (HSCT) consolidation for the treatment of r/r T-ALL? What are your team’s future research plans for this approach?
Prof. Pan Jing: Over the past three years of research data, we observed two key phenomena: First, regarding the issue of off-tumor target relapse in CAR-T therapy, especially the phenomenon observed in CD7 CAR-T treatment, CD5 CAR-T provided an effective complementary approach. Therefore, I believe that the current position of CD5 CAR-T in the treatment field is primarily as a supplement for patients who have failed CD7 CAR-T therapy. However, in cases of T-ALL relapse, if the patient’s CD5 expression is superior to CD7, the use of CD5 CAR-T can also be considered. From a safety perspective, using it as a bridge to transplantation is relatively safe. In the future, we may further explore the application of CD5 CAR-T, not only as a salvage measure but also based on the patient’s expression profile to select the most suitable CAR-T target.
Secondly, we noticed that patients treated with CD5 CAR-T therapy exhibited differences in immune reconstitution compared to those treated with CD7 CAR-T therapy. In normal individuals, approximately 10% of T cells are CD7 negative. During T cell reconstitution, especially in the absence of transplantation, CD7 negative T cells tend to self-renew and reconstitute more rapidly. However, after CD5 CAR-T therapy, patients almost lack normal CD5 negative cells. In another study on virus reactivation that we reported at this meeting, we found that among long-term follow-up CD5 CAR-T remission patients, the majority of their CD5 negative cells exhibited very slow growth, and these cells mostly originated from the knockdown results in the CAR-T product, with poorer function compared to normal CD7 negative T cells. Based on this finding, we recommend that patients should undergo bridging transplantation after CD5 CAR-T therapy to facilitate immune reconstitution. This is because the lack of normal CD5 negative T cells may pose a serious risk of infection. This is another important message that we hoped to convey through our presentation at this meeting.
Abstract No.: S305
CMV/EBV INFECTIONS IN CAR-T THERAPY FOR RELAPSED/REFRACTORY T-CELL ACUTE LYMPHOBLASTIC LEUKEMIA/LYMPHOMA
Background
Recently, chimeric antigen receptor (CAR) T cell therapies targeting CD7 or CD5 have shown efficacy in patients with relapsed/refractory T-cell acute lymphoblastic leukemia/lymphoma (r/r T-ALL/LBL). However, severe infections, particularly cytomegalovirus (CMV) and Epstein-Barr virus (EBV) infections, remain a major risk during treatment, which may be related to the depletion of non-malignant T cells mediated by CAR-T cells.
Aim
This study aims to summarize the CMV and EBV infections in patients receiving CD7 or CD5 CAR-T cell therapy and provide some risk management strategies.
Methods
This study is based on data from a phase I trial of autologous CD7 CAR-T therapy (NCT04840875), a phase I (ChiCTR2000034762) and phase II trial (NCT04689659) of donor-derived CD7 CAR-T therapy, and a phase I trial of donor-derived CD5 CAR-T therapy (NCT05032599). All patients or their guardians provided written informed consent prior to screening. Infections were graded according to CTCAE version 5.0. Single factor analysis was performed using non-parametric tests, and multifactor analysis was performed using logistic regression analysis.
Results
From July 2020 to September 2023, the study enrolled a total of 114 patients. 25 (22%) had CMV infections, 17 (15%) had EBV infections, and 6 had concurrent CMV and EBV infections.
Within 30 days after CAR-T cell infusion, 2 (2%) grade 1 CMV infections and 2 (2%) grade 1 EBV infections were observed. After 30 days of infusion, 107 patients continued follow-up (7 patients dropped out of the trial). Among the 65 patients who did not receive consolidative SCT, 14 (22%) had their total T cell counts (53 CD5+CD7-, 8 CD5-CD7+, 4 CD5-CD7-) recover to normal levels at a median time of 1.3 months (IQR, 0.8~2.8) after infusion, and 18 (28%) had their CD4+ lymphopenia recover to grade 2 or lower at a median time of 3.2 months (IQR, 2~4.3) after infusion. Of these, 16 (25%) developed CMV infections (6 severe) at a median of 2 months (IQR, 1.3~3.3) after infusion, and 8 (12%) developed EBV infections (4 severe) at a median of 1.1 months (IQR, 0.8~1.3) after infusion.
In the 42 patients who received SCT, 9 (21%) had their total T cell counts (26 CD5+CD7+, 13 CD5+CD7-, 3 CD5-CD7+) recover to normal levels at a median time of 6.2 months (IQR, 3.7~8) after transplant, and 16 (38%) had their CD4+ lymphopenia recover to grade 2 or lower at a median time of 2.6 months (IQR, 0.9~4.6) after transplant. Of these, 7 (17%) developed CMV infections (1 severe) at a median of 1.1 months (IQR, 0.8~1.3) after SCT, and 7 (17%) developed EBV infections (4 severe) at a median of 2.1 months (IQR, 1.2~2.7) after SCT.
Almost all patients experienced T cell and CD4+ T cell deficiencies, which may be one of the causes of infections. The median total T cell count and CD4+ T cell count at day 30 after infusion were 135/μL (IQR, 31~259) and 15/μL (IQR, 9~22), respectively, in infected patients, lower than 302/μL (IQR, 36~616) (P=0.036) and 79/μL (IQR, 20~145) in non-infected patients.
Furthermore, we observed that the peak CAR-T cell expansion was higher in CD5 CAR-T therapy than in CD7 CAR-T therapy (P=0.012), while the peak CAR-T cell expansion was comparable between infected and non-infected patients (P=0.362). 11 patients had detectable CAR-T cells after transplant, and 7 of them had viral infections, indicating that infections occurring after SCT may also be related to the persistence of CAR-T cells.
Through multifactor analysis of these variables, including the absolute peak of CAR-T cell expansion, total T cell count at day 30, and CD4+ T cell count at day 30, we found that total T cell deficiency at day 30 was independently associated with viral infections (P=0.029).
Conclusions
Most patients receiving CD5 and CD7 CAR-T cell therapy experience T cell deficiencies that are difficult to recover. The study found that T cell deficiency is an independent risk factor for viral infections. Therefore, consolidative transplantation is recommended after CAR-T cell therapy to promote T cell recovery. Additionally, total T cells usually recover within 6 months after SCT, so there is still a risk of infection in the early period after SCT. Some infections occurring after SCT may be related to the persistence of CAR-T cells, and implementing a reliable “suicide switch” in the CAR-T product may improve the safety of CAR-T cell therapy for T-ALL in future studies.
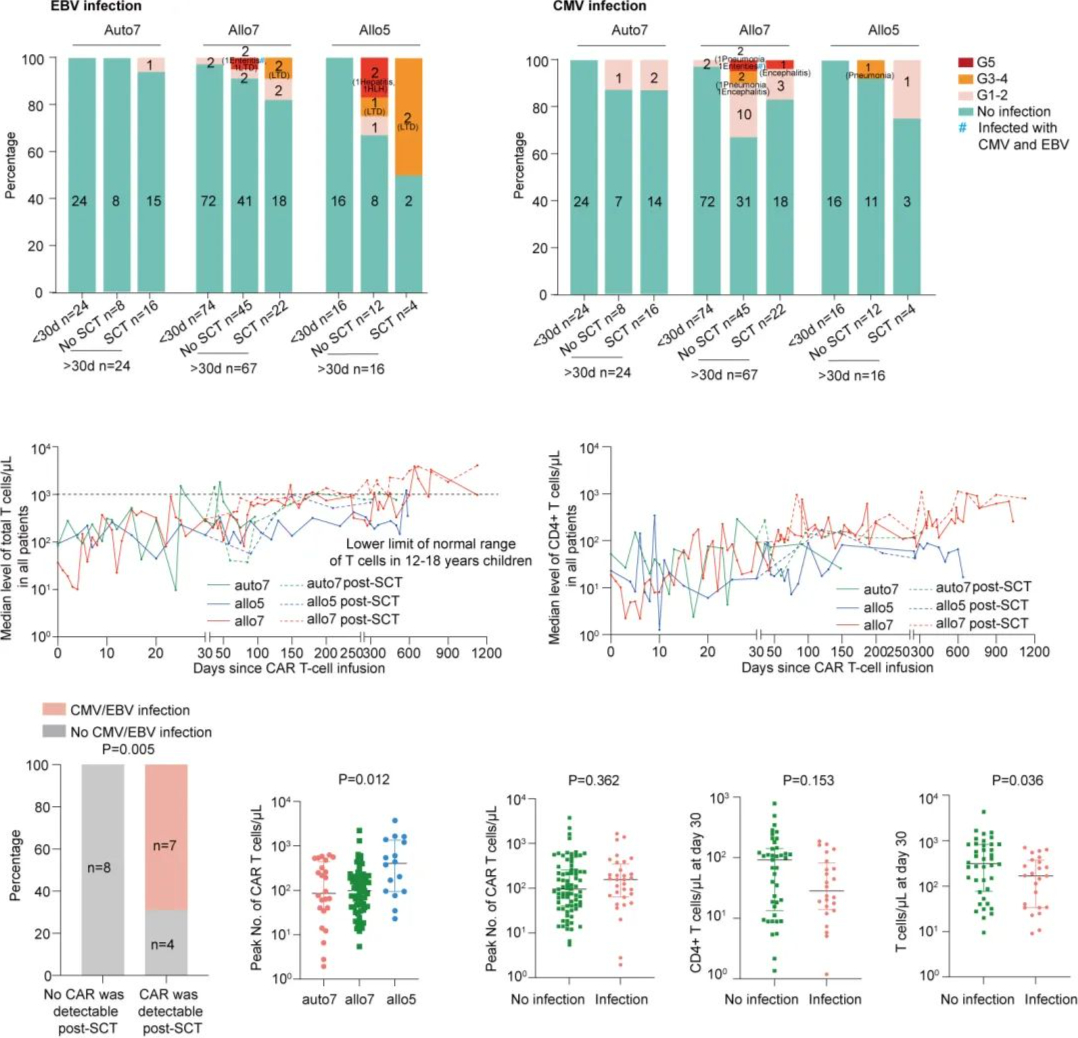
Figure 2. EBV and CMV infections, T cell and CD4+ T cell levels after CAR-T cell infusion
Expert Interview
Tumor Outlook – Hematology Express
Another study explored CMV/EBV infections in CAR-T therapy for relapsed/refractory acute T-cell lymphoblastic leukemia/lymphoma. Could you please introduce how many patients developed CMV and EBV infections in the study? At what stage did these infections typically occur after CAR-T cell infusion? What risk management strategies did your team provide for these infections?
Professor Pan Jing: In fact, this study is part of the same series as the CD5 CAR-T study we mentioned above and the previously published CD7 CAR-T studies. Currently, the main challenge in this field is to verify whether these drugs are effective for r/r T-ALL and whether they can serve as standalone drugs without the need for bridging transplantation to achieve cure. To answer these questions, we need to follow up with patients for an extended period and evaluate their T cell function. In this CAR-T therapy for T-ALL study, we reviewed four studies, three involving CD7 CAR-T and one involving CD5 CAR-T, with a total of 114 patients enrolled. About half of these patients underwent bridging transplantation.
Firstly, we focused on the risks to patients during the CAR-T therapy response period (within 30 days). Based on our data and data from other centers in China, the safety during this period is relatively high. Among the 114 patients, only 3 developed infections, which were mild and rapidly resolved with antiviral treatment. Further analysis showed that patients in the bridge-to-transplant group, including those receiving second transplants, had an overall higher risk of infection, as their immune system takes about six months to reconstitute after transplantation. In contrast, patients in the non-bridge-to-transplant group, especially those with severe hematological toxicity before treatment, were more prone to severe infections after 30 days of CAR-T therapy. This is because severe infections require both an immune deficiency and time to develop.
Our long-term follow-up data showed that T-cell function recovery in non-bridge-to-transplant patients was very slow, potentially taking about a year to approach the levels after CD19 CAR-T therapy. Therefore, for patients with very low blood counts and severe hematological toxicity after CD7 CAR-T or CD5 CAR-T therapy, we recommend early bridge-to-transplant to promote rapid T-cell reconstitution and avoid infections. For patients after CD5 CAR-T therapy, we particularly recommend immediate bridge-to-transplant, as the patient’s CD5-negative T cells mainly originate from the CAR-T product. To this end, we may consider separating the CD5 CAR-T product into CAR-T and CD5-negative T cells, and supplementing patients with sufficient CD5-negative T cells to support their immune reconstitution. This could be a future research direction for us.
Tumor Outlook – Hematology News
In your study, you observed that infections after stem cell transplantation (SCT) might be related to the persistence of CAR-T cells. How might this finding impact the safety of future CAR-T therapies? What is your opinion on the necessity of implementing a “suicide switch” technology in CAR-T products?
Professor Pan Jing: This phenomenon has been observed not only at our center but also at multiple centers across the country. T-cell CAR-T therapy has been implemented for nearly two to three years, and large transplant institutions like ours often communicate and share our experiences. One issue we’ve identified is that if patients do not undergo a bridge-to-transplant, for example, after completing CD7 CAR-T therapy and receiving an autologous stem cell infusion, the CAR-T cells almost never decrease. In this situation, patients may face a high risk of viral reactivation and sepsis in the later stages. Our team also presented a detailed report on this at the recent EHA meeting.
For patients undergoing bridge-to-transplant, according to the traditional concept of CD19 CAR-T therapy, we expected that the donor stem cells after standard transplantation and conditioning would eliminate the CAR-T cells. However, this is not always the case, as not all CAR-T cells disappear. For instance, at yesterday’s Poster Session, Professor Su Yi’s team from the Western Theater General Hospital in China presented data showing that a small number of patients still had CAR-T cells after transplantation. Our center, as well as other transplant centers in Chengdu, Shanghai, and Wuhan, have also observed this phenomenon. These patients experience severe immune deficiencies later on. Therefore, we urge that for post-transplant patients, especially at less experienced transplant centers, it is essential to test the patients’ T-cell phenotypes after transplantation. This is because only 48% of patients have their T cells recover to a normal CD7 and CD5 double-positive state one month after transplantation, indicating that T-cell recovery is a slow process. If T cells do not recover normally, the patient’s risk of infection will significantly increase.
Additionally, although we have not yet obtained complete data on the choice of transplant conditioning regimens, we have observed that patients receiving total body irradiation (TBI) have a lower likelihood of CAR-T cell survival after transplantation. In contrast, patients receiving non-TBI regimens have a relatively higher rate of CAR-T cell survival. This is the result of our private communications among several centers. As for how to make bridge-to-transplant safer, we believe further support from large datasets is needed. In our clinical trials of T-cell CAR-T therapy, we attempted to use switches to control the function of CAR-T cells, but unfortunately, all reported switch methods have been ineffective so far. Therefore, our next focus is to develop a more suitable and clinically effective switch to rapidly turn off CAR-T function when a patient develops an infection, restoring their normal immune function and reducing the risk of infection. This will be the subject of our subsequent basic and translational research.
Content Source:肿瘤瞭望–血液时讯
