CAR-T Non-Hodgkin’s Lymphoma, Voice from China at EHA | Prof. Jia Yi’s Team: Superiority of CD19/20 Bispecific CAR-T Therapy in Treating Patients with Relapsed/Refractory B-Cell Lymphoma
CAR-T Non-Hodgkin’s Lymphoma, Voice from China at EHA | Prof. Jia Yi’s Team: Superiority of CD19/20 Bispecific CAR-T Therapy in Treating Patients with Relapsed/Refractory B-Cell Lymphoma
The 29th Annual Congress of the European Hematology Association (EHA) was held in Madrid, Spain, from June 13 to 16, 2024. As the largest international conference in the field of hematology in Europe, it attracts experts and scholars from around the world every year to share and discuss innovative ideas and the latest scientific and clinical research results in hematology. At this year’s congress, Prof. Jia Yi’s team from Tongji Hospital, Huazhong University of Science and Technology, had multiple studies selected for poster or e-poster presentation. This report focuses on two studies (P2090, P1164) in the field of aggressive B-cell lymphoma, aiming to provide insights into improving long-term survival and optimizing treatment choices for patients with relapsed/refractory B-cell lymphoma.

Serum Eotaxin Predicts Long-Term Survival of Patients with Relapsed/Refractory Aggressive B-Cell Lymphoma Receiving CD19 CAR-T Therapy
Research Background
Non-Hodgkin’s lymphoma (NHL) is a common life-threatening malignancy in China. Recent clinical trials of chimeric antigen receptor T-cell (CAR-T) therapy have significantly improved the prognosis of B-cell tumors. CD19-targeted third-generation CAR-T therapy has become an important treatment for refractory/relapsed lymphoma, especially B-cell tumors, but challenges such as poor efficacy and post-treatment relapse still exist. Therefore, early identification of patients with non-response or high risk of relapse through clinical characteristics and biomarkers is crucial. Understanding the timing and susceptibility factors of relapse can further enhance the effectiveness of CD19 CAR-T therapy.
Research Objective
To predict CAR-T durability and patient long-term prognosis based on cytokine profiling.
Research Methods
We enrolled 44 patients diagnosed with refractory or relapsed aggressive B-cell lymphoma from December 2017 to November 2022. These patients received commercial CD19 CAR-T products or participated in clinical trials involving CD19 CAR-T therapy. A total of 88 serum samples were collected before CAR-T infusion (day 0) and on day 7 or 14 after infusion. Serum samples were analyzed using the meso scale discovery and luminex methods. A p-value less than 0.05 was considered statistically significant.
Research Results
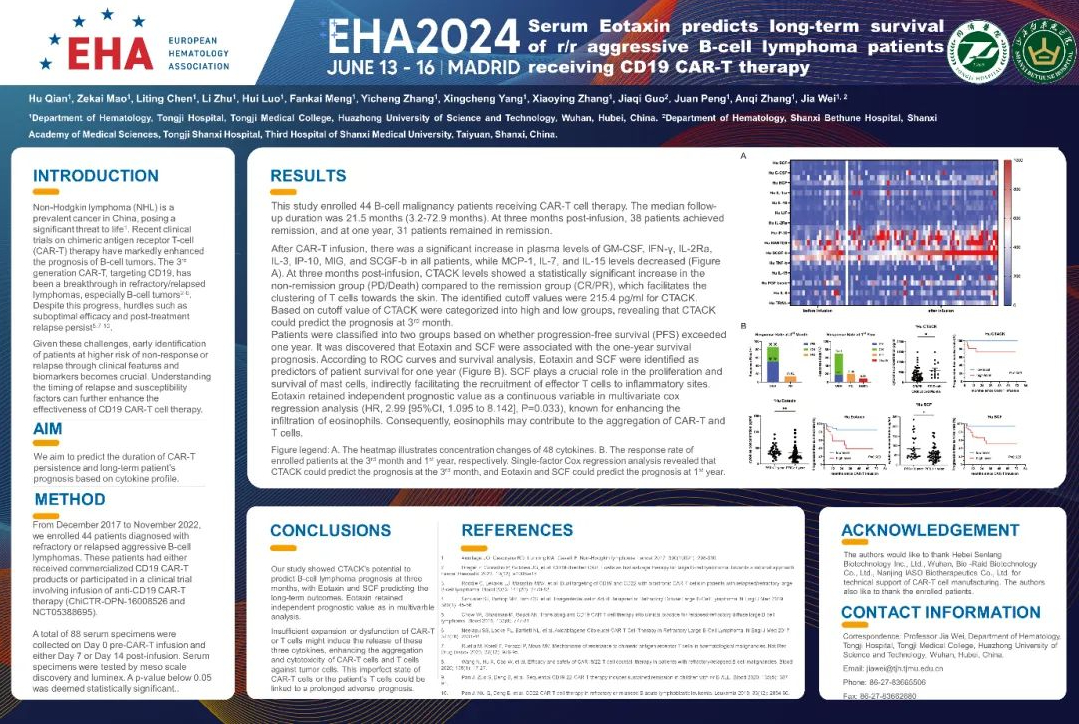
This study recruited 44 patients with B-cell malignancies receiving CAR-T therapy. The median follow-up time was 21.5 months (range: 3.2-72.9 months). At 3 months post-infusion, 38 patients achieved remission, and 31 patients maintained remission at 1 year. After CAR-T infusion, plasma levels of GM-CSF, IFN-γ, IL-2 Ra, IL-3, IP-10, IL-10, and SCGF-b were significantly increased in all patients, while levels of MCP-1, IL-7, and IL-15 decreased. At 3 months post-infusion, CTACK levels were significantly higher in the non-remission group (PD/death) compared to the remission group (CR/PR), and CTACK can promote T-cell trafficking to the skin. We determined the cutoff value of CTACK as 215.4 pg/ml based on the ROC curve. Patients were divided into high and low CTACK level groups according to the cutoff value, and the results suggested that CTACK could predict the 3-month prognosis. Patients were divided into two groups based on whether progression-free survival (PFS) exceeded one year. The study found that Eotaxin and SCF were associated with the 1-year survival prognosis. According to the ROC curve and survival analysis, Eotaxin and SCF were identified as predictors of 1-year patient survival (Figure B). SCF plays a crucial role in mast cell proliferation and survival, indirectly promoting the recruitment of effector T cells to inflammatory sites. In the multivariate Cox regression analysis, Eotaxin was an independent risk factor for long-term patient survival (P=0.033). Eotaxin can promote eosinophil infiltration. Therefore, eosinophils may facilitate the recruitment of CAR-T and T cells.
Research Conclusion
Our study shows that the CTACK level at 3 months has the potential to predict the prognosis of patients receiving CD19 CAR-T therapy, while Eotaxin and SCF levels are associated with 1-year prognosis after treatment. High Eotaxin levels were an independent risk factor for long-term prognosis in the multivariate analysis. Insufficient expansion or functional impairment of CAR-T or T cells may induce the release of these three cytokines, enhancing the recruitment and cytotoxicity of CAR-T cells and T cells against tumor cells, which is unfavorable for long-term patient prognosis.
Superiority of CD19/20 Bispecific CAR-T Therapy in Treating Patients with Relapsed/Refractory B-Cell Lymphoma: A Preliminary Interim Report from a Multicenter Study
Research Background
CD19 chimeric antigen receptor T-cell therapy has shown significant efficacy in patients with B-cell lymphoma and B-cell acute lymphoblastic leukemia. However, its efficacy is limited due to CD19 antigen loss or downregulation. In phase 1-2 CD19 CAR-T clinical trials, the median progression-free survival was only 5.9 months. Studies have found that simultaneously targeting two antigens with CAR-T cells can reduce the risk of disease relapse, such as CD19/22 bispecific CAR-T cells, which have shown excellent efficacy against B-cell malignancies. The CD20 antigen is widely expressed on malignant B cells, and CD20 monoclonal antibodies have become the standard treatment for diffuse large B-cell lymphoma, follicular lymphoma, and chronic lymphocytic leukemia. These findings led us to explore whether CD19/20 bispecific CAR-T therapy would have an advantage. Therefore, we used second-generation CAR-T cells targeting CD19/20 to treat patients with relapsed/refractory B-cell lymphoma from three centers.
Research Objective
In this study, our objective was to develop CD19/20 bispecific CAR-T cells and evaluate their safety and efficacy in treating patients with relapsed/refractory B-cell lymphoma.
Research Methods
In this study, from July 2022 to December 2023, 16 patients with relapsed/refractory B-cell lymphoma (DLBCL, n=11; BCL, n=1; MZL, n=2; BL, n=2) received CD19/20 bispecific CAR-T therapy (2*106/kg, n=3; 3*106/kg, n=2; 4*106/kg, n=2; 5*106/kg, n=7; 6*106/kg, n=2). These patients were from Tongji Hospital, Shanxi Bethune Hospital, and the Fourth Hospital of Hebei Medical University.
Research Results
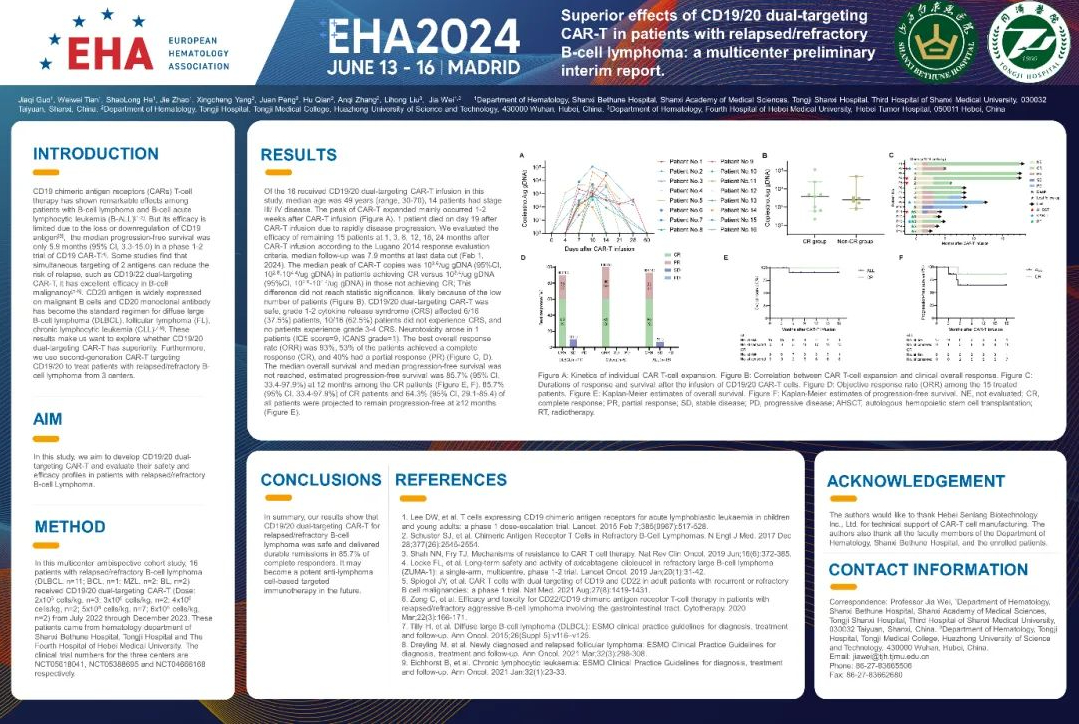
Among the 16 patients receiving CD19/20 bispecific CAR-T infusion in this study, the median age was 49 years (range: 30-70 years), and 14 patients had stage III/IV disease. The CAR-T expansion peak mainly occurred 1-2 weeks after CAR-T infusion (Figure A). One patient died on day 19 post-infusion due to rapid disease progression. We assessed the efficacy of the remaining 15 patients according to the Lugano 2014 response criteria at 1, 3, 6, 12, 18, and 24 months after CAR-T infusion, with a median follow-up time of 7.9 months (as of February 1, 2024). Among patients who achieved CR, the median peak CAR-T copy number was 103.6/ug gDNA (95% CI: 102.8-104.4/ug gDNA), while in non-CR patients, the median peak CAR-T copy number was 103.4/ug gDNA (95% CI: 102.9-104.7/ug gDNA); this difference was not statistically significant, likely due to the small number of patients (Figure B). CD19/20 bispecific CAR-T therapy was safe, with 6/16 (37.5%) patients experiencing grade 1-2 cytokine release syndrome (CRS), and 10/16 (62.5%) patients did not experience CRS. No patients experienced grade 3-4 CRS. One patient developed neurotoxicity (ICE score=9, ICANS score=1). The overall response rate (ORR) was 93%, with 53% of patients achieving complete remission (CR) and 40% achieving partial remission (PR) (Figures C, D). The median overall survival and median progression-free survival for CR patients were not reached, and the estimated 12-month progression-free survival rate was 85.7% (95% CI: 33.4-97.9%) (Figures E, F). An estimated 85.7% (95% CI: 33.4-97.9%) of CR patients and 64.3% (95% CI: 29.1-85.4%) of PR patients maintained progression-free status at ≥12 months (Figure E).
Research Conclusion
In summary, our study results demonstrate that CD19/20 bispecific CAR-T therapy for relapsed/refractory B-cell lymphoma is safe, and 85.7% of complete responders achieved durable remission. It may become an effective targeted immunotherapy against lymphoma cells in the future.
Content Source:血液时讯
