The Revolutionary Transformation of BCMA CAR-T Multiple Myeloma
The Revolutionary Transformation of BCMA CAR-T Multiple Myeloma
Multiple myeloma (MM) is the second most common hematological malignancy in both China and the United States. Over the past decade, the emergence of several novel therapies has significantly improved patient survival rates. Among them, CAR-T therapy, as the latest treatment modality, has brought about a revolutionary change in the treatment of MM.
About Multiple Myeloma
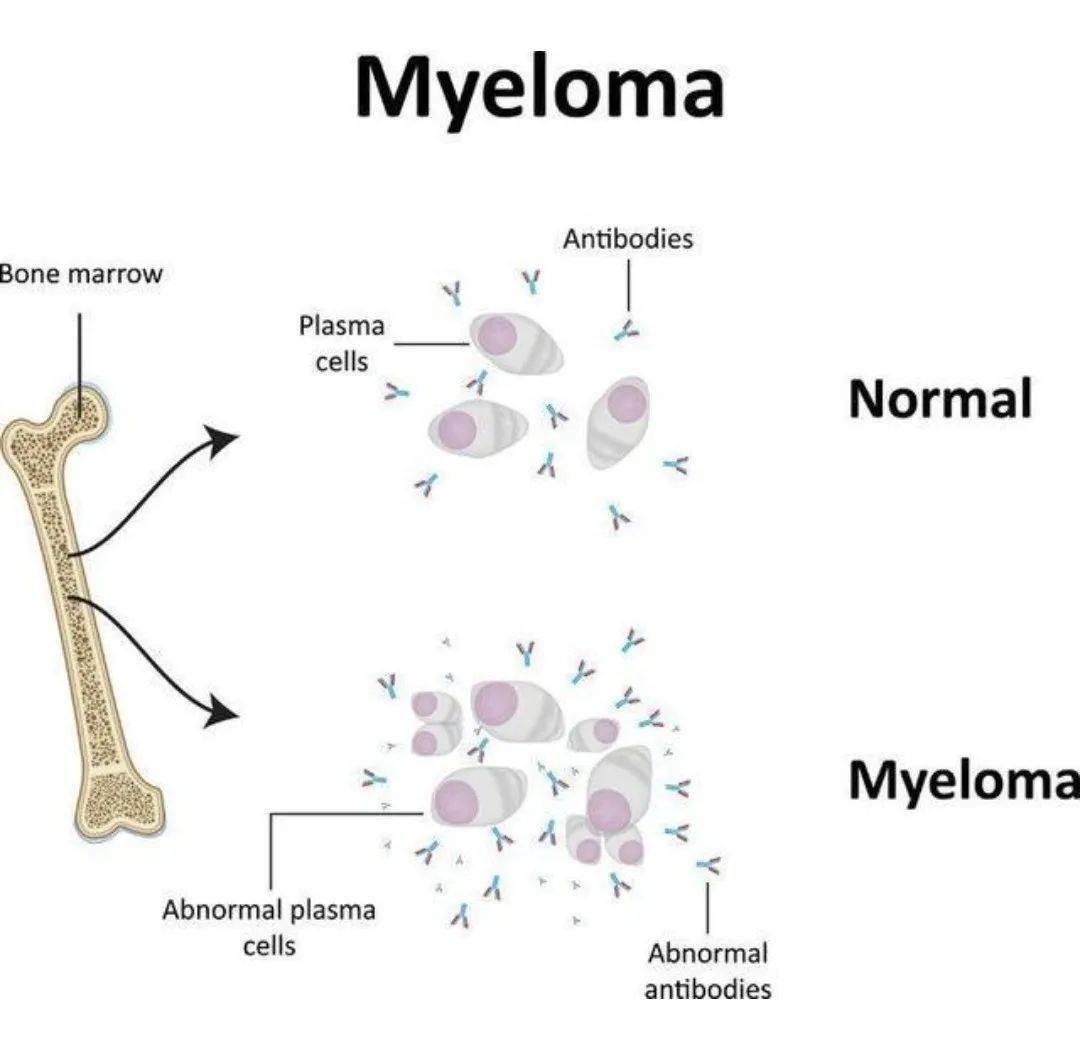
Multiple myeloma (MM) is a hematological malignancy characterized by the clonal proliferation of plasma cells in the bone marrow and the overproduction of monoclonal immunoglobulins, leading to impaired hematopoietic function, bone destruction, and renal impairment. In both the United States and China, MM is the second most common hematological malignancy. It is estimated that in 2023, there will be 35,730 new cases of MM and 12,590 MM-related deaths in the United States, while in China, the number of new MM cases is estimated to be 23,200. MM is more prevalent in the elderly population. MM is considered incurable, and most patients experience an initial remission after treatment but eventually relapse and may develop refractory disease. Generally, the duration of remission shortens as the number of treatment lines increases.
Research Progress and Application Status of CAR-T Therapy in MM
Over the past 20 years, the main treatment drugs for MM have been proteasome inhibitors (PIs) (e.g., Bortezomib, Ixazomib, and Carfilzomib), immunomodulatory drugs (IMiDs) (e.g., Thalidomide, Lenalidomide, and Pomalidomide), and CD38 monoclonal antibodies (e.g., Daratumumab). Unfortunately, after undergoing various combination regimens with these drugs, patients typically develop resistance within 6-10 years after diagnosis, making subsequent treatment very challenging. The advent of CAR-T therapy has changed the situation for these patients.
In recent years, clinical trials have demonstrated the remarkable efficacy of CAR-T therapy in relapsed/refractory MM (RRMM). Currently, two BCMA-targeted CAR-T therapies, idecabtagene vicleucel (ide-cel; trade name: Abecma) and ciltacabtagene autoleucel (cilta-cel; trade name: Carvykti), have been approved by the FDA in 2021 and 2022, respectively, for the treatment of RRMM in patients who have received at least five prior lines of therapy. The approvals were based on two single-arm studies: KarMMa and CARTITUDE-1. In the KarMMa study, patients who had received ≥4 prior lines of therapy had an objective response rate (ORR) of 72% and a complete response (CR) rate of 28%. In the CARTITUDE-1 study, these patients had an ORR of 97.9% and a stringent complete response (sCR) rate of 78.4%. The response rates and depth of response achieved were unprecedented compared to any previous therapies.
The phase III KarMMa-3 and CARTITUDE-4 trials have further advanced CAR-T therapy to earlier lines of RRMM, with both studies meeting their primary endpoint of progression-free survival (PFS). The KarMMa-3 study enrolled RRMM patients who had received 2-4 prior lines of therapy (including IMiD, PI, and anti-CD38 antibody). At a median follow-up of 18.6 months, the median PFS was 13.3 months in the ide-cel group versus 4.4 months in the standard of care (SOC) group (HR=0.49, P<0.0001); at a median follow-up of 30.9 months, the median overall survival (OS) was 41.4 months versus 23.4 months. The CARTITUDE-4 study included MM patients who had received 1-3 prior lines of therapy (including PI and IMiD) and were lenalidomide-refractory. The results showed that the median PFS was not reached in the cilta-cel group versus 11.8 months in the SOC group (HR=0.41, P<0.0001).
Based on the results of these two phase III studies, the sponsors submitted supplemental Biologics License Applications (sBLAs) to the FDA to expand the indications to earlier lines of treatment: ide-cel for adult RRMM patients who have received IMiD, PI, and anti-CD38 antibody therapy; cilta-cel for adult RRMM patients who have received at least one prior line of therapy (including PI and IMiD) and are lenalidomide-refractory. Noting an increased risk of early death in the treatment arms of both studies, the FDA convened two ODAC meetings on March 15, 2024, to discuss and vote on whether the benefit-risk profiles of these two drugs for the proposed indications were favorable. Ultimately, ide-cel and cilta-cel received favorable votes from the ODAC committees, with 8:3 and 11:0 votes, respectively. It is expected that these two drugs will soon be formally approved by the FDA for use in earlier lines of RRMM.
As seen in other diseases, CAR-T therapy for MM is associated with two major toxicities: cytokine release syndrome and neurotoxicity, as well as other toxicities. However, as clinical experience with CAR-T therapy accumulates, the management of CAR-T-related toxicities has become increasingly mature, and toxicity is no longer an obstacle to the application of CAR-T therapy.
Furthermore, due to the potential risk of secondary malignancies (T-cell malignancies), CAR-T therapy has been given a black box warning by the FDA. However, the causal relationship between CAR-T therapy and T-cell malignancies is unclear, and the incidence is extremely low. At least for the foreseeable future, the benefits of CAR-T therapy will outweigh the risks.
The Future of CAR-T in MM
In the future, could CAR-T therapy advance to the first or second line of treatment for MM? In fact, both the KarMMa-3 and CARTITUDE-4 studies included patients who had received earlier lines of therapy, including those who had received one or two prior lines of therapy. These earlier-line patients treated with CAR-T had better PFS and ORR compared to the SOC group, suggesting the potential for CAR-T therapy to move to earlier lines of treatment.
What remains unclear is whether every patient needs CAR-T therapy at the first relapse or whether we can more selectively determine which specific subgroups of patients at different lines of therapy could benefit more from CAR-T therapy. At what stage should CAR-T therapy be given to which patients? In fact, for newly diagnosed patients eligible for transplantation, there are ongoing randomized phase III clinical trials comparing CAR-T therapy with autologous stem cell transplantation. Even for patients who do not meet the transplant criteria, there are clinical trials exploring the possibility of using CAR-T therapy instead of prolonging maintenance and consolidation therapies.
It is certain that CAR-T therapy will advance to earlier lines of treatment.
CAR-T Therapies Approved for MM in China
Currently, two CAR-T therapies have been approved in China for the treatment of RRMM: Equecabtagene Autoleucel from IASO Bio, which received conditional approval from the National Medical Products Administration (NMPA) on June 30, 2023, for the treatment of adult RRMM patients who have progressed after at least three lines of therapy (including at least one PI and one IMiD); and Zevorcabtagene Autoleucel from CARsgen Therapeutics Holdings Limited, approved on March 1, 2024, for the treatment of adult RRMM patients who have progressed after at least three lines of therapy (including at least one PI and one IMiD). Both therapies target BCMA.
Assuming you are a professional medical translator proficient in medical knowledge and English-Chinese translation, capable of accurately translating medical terminology, now you need to use your expertise to accurately translate the above article into English. It is essential that medical terms are translated with precision, and the semantics are clear.
