Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Chinese ADC Drug Targeting B7-H3 Approved for Clinical Trials!
Chinese ADC Drug Targeting B7-H3 Approved for Clinical Trials!

ADC
#ADC #Immunotherapy#B7H3 #LungCancer #HeadAndNeckCancer #ADCDrug
On September 20, the China National Medical Products Administration (NMPA) approved BeiGene’s innovative anti-cancer drug, BGB-C354, for clinical trials. This exciting news marks the first approval for clinical research of this novel molecule in China. BGB-C354 is an Antibody-Drug Conjugate (ADC) specifically designed to target B7-H3, a protein often overexpressed in various cancers such as lung cancer, prostate cancer, breast cancer, and squamous cell carcinoma of the head and neck.
BGB-C354 holds significant promise for treating patients with advanced solid tumors, particularly lung cancer and head and neck squamous cell carcinoma (HNSCC). B7-H3 has gained attention as a key anti-cancer target, with its high expression often linked to poor prognosis. By leveraging the power of ADC technology, BGB-C354 aims to selectively deliver potent anti-cancer drugs directly to tumor cells, minimizing damage to healthy cells.
BeiGene has already initiated a Phase 1 clinical trial in the US and Australia, evaluating the safety, tolerability, and preliminary anti-tumor activity of BGB-C354 as a monotherapy and in combination with anti-PD-1 antibody, Tislelizumab. This recent approval sets the stage for the commencement of clinical trials in China.
Globally, B7-H3-targeted therapies are advancing rapidly. Companies like Daiichi Sankyo, Merck, and GSK are pushing the boundaries with their ADCs, entering Phase 2 and 3 clinical trials. The approval of BGB-C354 marks a significant step in advancing cancer treatment options in China, offering new hope for patients with difficult-to-treat cancers.
To assess whether the condition is suitable for clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
WhatsApp: +8613717959070
Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#CancerTreatment #ClinicalTrials #BeiGene #OncologyBreakthrough #PharmaInnovation #CancerResearch
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79
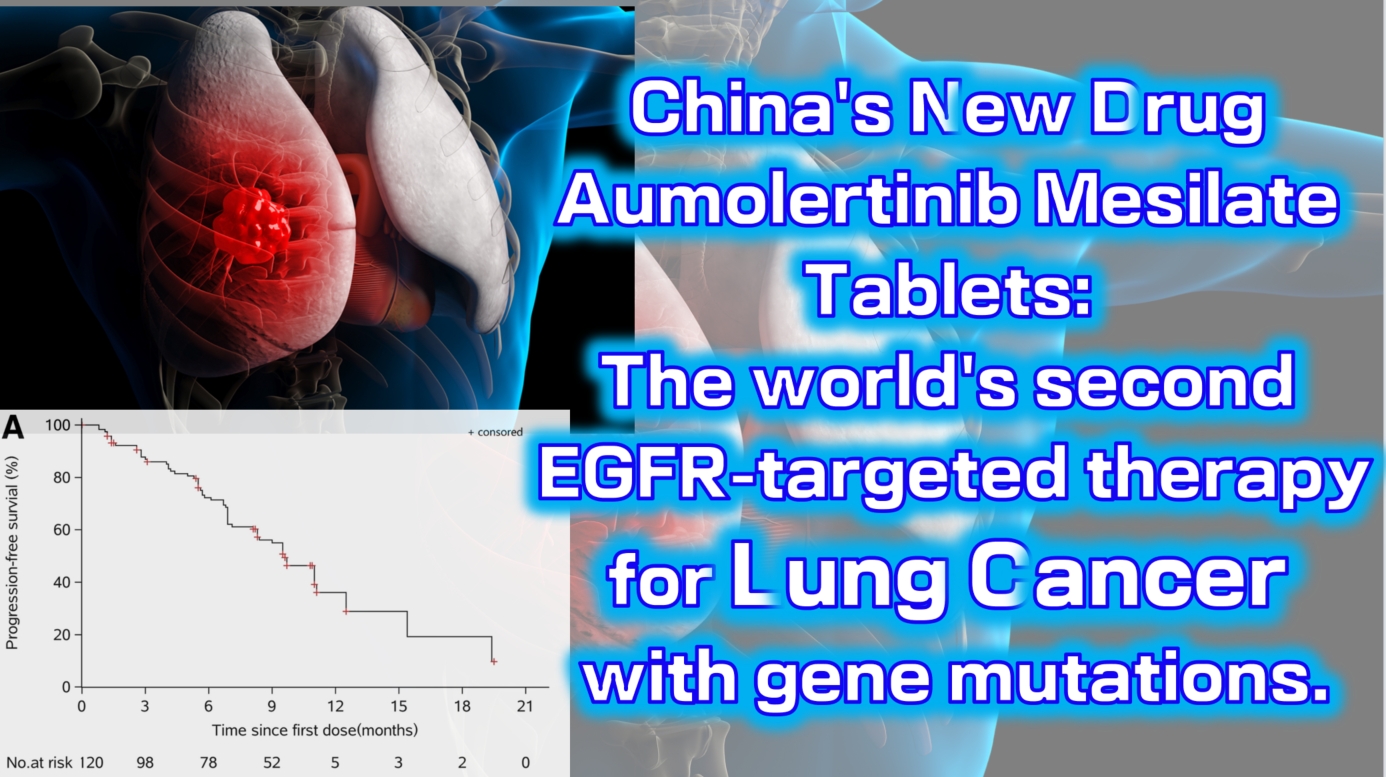
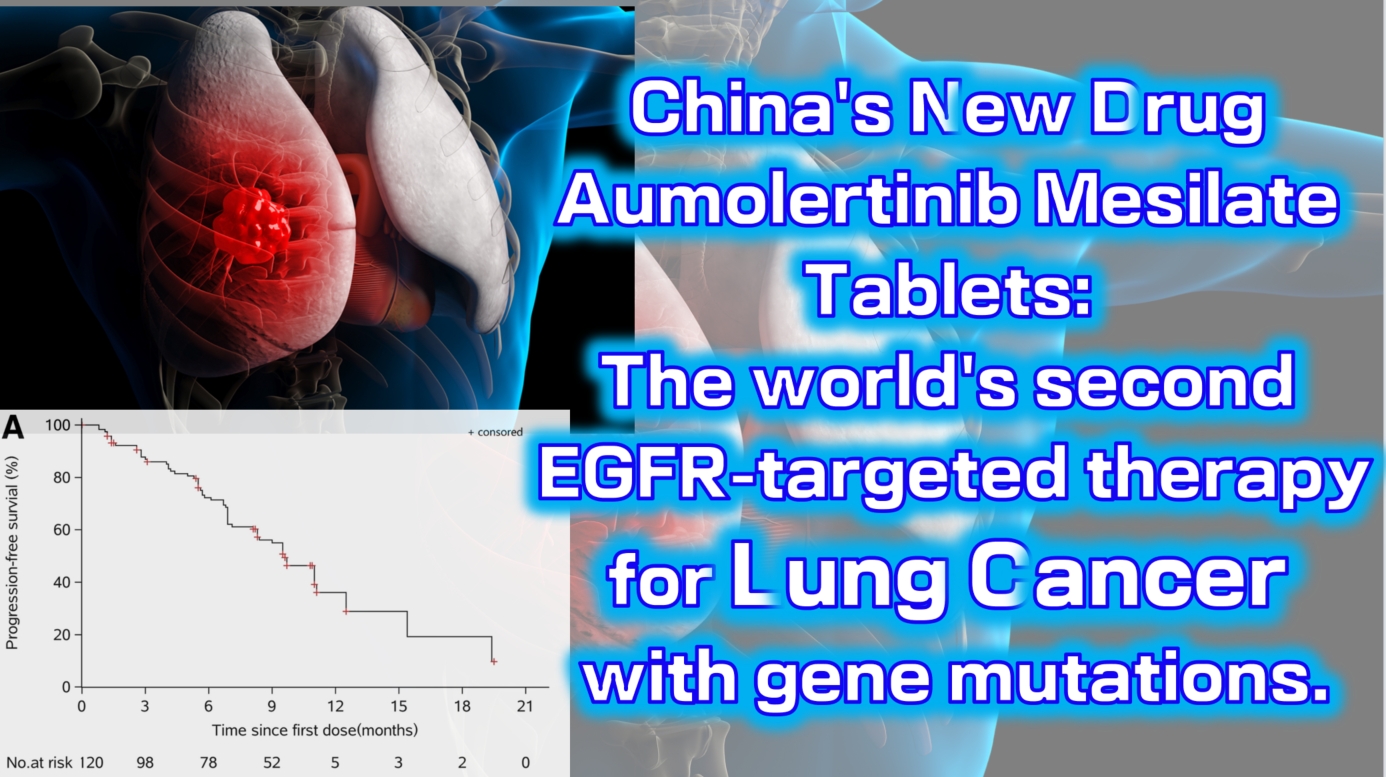
China’s new drug Aumolertinib Mesilate Tablets: The world’s second EGFR-targeted therapy for lung cancer with gene mutations.
China’s new drug Aumolertinib Mesilate Tablets: The world’s second EGFR-targeted therapy for lung cancer with gene mutations.
lung cancer
#LungCancer #EGFRInhibitor #TargetedTherapy #Aumolertinib #NSCLC
Aumolertinib Mesilate Tablets (Ameile) were approved for marketing in China on March 18, 2020. It is China’s first third-generation EGFR-targeted therapy for lung cancer with gene mutations and the second such drug globally, following Osimertinib.
On August 20, 2024, the new indication marketing application for Aumolertinib Mesilate Tablets was accepted for priority review by the China Center for Drug Evaluation (CDE). This indication is for the treatment of unresectable locally advanced non-small cell lung cancer (NSCLC) that has not progressed following platinum-based chemoradiotherapy. This is the fourth indication for which the drug has submitted a marketing application, and it is expected to be approved in the second quarter of 2025.
The Phase 1 clinical trial (NCT0298110) enrolled a total of 120 patients with locally advanced or metastatic non-small cell lung cancer (NSCLC). The results showed an objective response rate (ORR) of 52% (range: 42–63), with a disease control rate (DCR) as high as 92% (range: 84–96). The median progression-free survival was 11.0 months (95% CI: 9.5-not reached).

 To assess whether the condition is suitable for CAR-T or clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
To assess whether the condition is suitable for CAR-T or clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
WhatsApp: +8613717959070
Email: doctor.huang@globecancer.com
#CancerTreatment #ClinicalTrials #PharmaInnovation #Oncology #DrugApproval #Biotech #PrecisionMedicine
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

**Chinese Biopharmaceuticals: Ushering in a New Era in Nasopharyngeal Carcinoma Treatment, EBV-Specific CAR-T Injection Approved for Phase II Clinical Trials in the US and China**
**Chinese Biopharmaceuticals: Ushering in a New Era in Nasopharyngeal Carcinoma Treatment, EBV-Specific CAR-T Injection Approved for Phase II Clinical Trials in the US and China**

Nasopharyngeal Carcinoma
#Nasopharyngeal #Carcinoma #BRG01 #CART #EBVspecific
Biosyngen has announced a milestone achievement: the company’s independently developed BRG01 injection (EBV-specific CAR-T) has received formal written approval from the U.S. Food and Drug Administration (FDA) to conduct pivotal Phase II clinical trials for the treatment of relapsed/metastatic EBV-positive nasopharyngeal carcinoma patients. This is the world’s first original cell drug for solid tumors approved in both the US and China to enter Phase II trials, bringing hope and breakthroughs to the field of solid tumor treatment.
Previously reported, the Center for Drug Evaluation (CDE) of the National Medical Products Administration has agreed to conduct pivotal Phase II clinical trials of BRG01 injection (EBV-specific CAR-T). Patients for the BRG01 US-China Phase I clinical trials completed enrollment by the end of January this year, and all trial participants have received BRG01 reinfusion treatment. The Phase I registered clinical trial of BRG01 has successfully completed DLT (dose-limiting toxicity) observation and efficacy evaluation in 9 patients, all of whom were advanced nasopharyngeal carcinoma patients who had failed at least one treatment, including PD-1 antibody immune checkpoint inhibitors.
The data shows that BRG01 has demonstrated excellent safety and preliminary efficacy: in PET-CT scans, 75% of high-dose patients experienced a local reduction in tumor lesions and a decrease in metabolic activity, with some patients achieving 100% complete remission of tumor lesions. Additionally, BRG01 also demonstrated excellent anti-EB virus efficacy, with a significant reduction of EB virus load in the peripheral blood of patients after reinfusion to normal levels.
These data not only highlight the potential of BRG01 in tumor treatment but also demonstrate its dual advantages in antiviral therapy, laying a solid foundation for future clinical applications. This is believed to be the key reason for the FDA’s approval of BRG01 to enter Phase II clinical trials.
The FDA’s approval not only highly recognizes the preliminary research results of BRG01 injection but also fully affirms Biosyngen’s innovative capabilities and research and development strength in the field of cellular immunotherapy. Biosyngen will take this as an opportunity to accelerate the clinical research process of BRG01 injection, striving to achieve the commercialization of this therapy as soon as possible to bring benefits to nasopharyngeal carcinoma patients worldwide.
Biosyngen’s layout in the field of solid tumor cell therapy goes far beyond this. The company has become a biotech enterprise with three major cellular therapies for both solid and hematological tumors: CAR-T, TCR-T, and TIL. The product pipelines have completed dual submissions and approvals in both the US and China, and the indications for the latter two include a variety of solid tumors such as lung and liver cancer.
Looking to the future, with Biosyngen’s efficient execution and rapid R&D achievements, we have reason to expect more clinical breakthroughs in solid tumor cell drugs in a shorter time, bringing new treatment hopes to patients.
🎉🎉To assess whether the condition is suitable for CAR-T or clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
WhatsApp: +8613717959070
Email: doctor.huang@globecancer.com
#Biosyngen #CAR_T #CancerTreatment #NasopharyngealCarcinoma #FDAApproval #ClinicalTrials #MedicalBreakthrough #BiotechInnovation #CancerResearch #Immunotherapy #HealthcareInnovation #CancerHope #SolidTumors #GlobalHealth #CancerCare
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79
Chinese Medical Team Research: 64.6% Complete Remission Rate, Over Half of Patients Progression-Free for More Than Two Years! Targeted Therapy Combined with Chemotherapy is Safe and Effective as First-Line Treatment for Lymphoma
**Chinese Medical Team Research: 64.6% Complete Remission Rate, Over Half of Patients Progression-Free for More Than Two Years! Targeted Therapy Combined with Chemotherapy is Safe and Effective as First-Line Treatment for Lymphoma**
Lymphoma
Peripheral T-cell lymphoma (PTCL) is a group of highly aggressive and heterogeneous diseases with poor prognosis. The standard CHOP regimen (cyclophosphamide, doxorubicin, vincristine, and prednisone) is widely used as first-line treatment for PTCL. Previous studies have confirmed the safety and efficacy of combining various targeted drugs with CHOP (CHOPX) for PTCL treatment. However, there are multiple PTCL subtypes with different mutations, such as TP53, TET2, KMT2D, and CREBBP/EP300, and evidence is still lacking regarding the effectiveness of these combined treatment regimens in patients with specific genetic mutations.
Recently, a Chinese study published in *The Lancet Regional Health–Western Pacific* showed that selecting targeted therapies based on specific genetic mutations, combined with CHOP as a first-line treatment for PTCL, demonstrated good efficacy and safety. Compared to standard CHOP, CHOPX treatment achieved a higher complete remission rate and longer progression-free survival. This study was conducted by a Chinese medical team.
This was an open-label, multi-center, non-randomized, external-controlled phase 2 clinical trial (code-named GUIDANCE-03) conducted across seven medical centers in China. The trial compared the efficacy and safety of targeted drug combinations based on specific genetic mutations with CHOP (CHOPX) versus CHOP alone in newly diagnosed PTCL patients.
A total of 96 newly diagnosed PTCL patients (aged ≥18 years, median age 63 years) were enrolled in the study, with 48 patients in each group (CHOPX and CHOP). Genetic sequencing results showed that 93 patients (96.9%) carried genetic mutations. Patients in the CHOPX group received standard CHOP treatment during the first treatment cycle. Starting from the second cycle, targeted drugs were added based on the patient’s specific genetic mutations: decitabine (for TP53 mutations), azacitidine (for TET2/KMT2D mutations), chidamide (for CREBBP/EP300 mutations), and lenalidomide (for patients without these mutations), with a total of six treatment cycles. Patients in the CHOP group received six cycles of CHOP treatment.
The primary endpoint of the study was the complete remission rate (CRR) at the end of treatment. Secondary endpoints included overall response rate (ORR), progression-free survival (PFS), overall survival (OS), and safety. The analysis results showed:
– At the end of treatment, the CRR of the CHOPX group was superior to that of the CHOP group. Compared to the CHOP group, the CHOPX group saw an approximate 30% improvement in CRR (64.6% vs. 33.3%, OR 0.27, 95% CI 0.12-0.64; P=0.004), achieving the primary endpoint of the study.
– For secondary endpoints, the ORR of the CHOPX group was better than that of the CHOP group (66.7% vs. 52.1%).
– During a median follow-up period of 24.3 months, the median PFS of the CHOPX group was significantly longer than that of the CHOP group (25.5 months vs. 9.0 months; HR 0.57, 95% CI 0.34-0.98; P=0.041), with a 43% reduction in the risk of disease progression or death. The 2-year PFS rates for the two groups were 53.2% (95% CI 38.7-67.7) and 28.0% (95% CI 13.6-42.3), respectively.
In terms of OS, the median OS for the CHOPX group has not yet been reached, while the median OS for the CHOP group was 30.9 months. The CHOPX group showed a trend toward improved OS, but the current statistical results are not significant (HR 0.55, 95% CI 0.28-1.10; P=0.088). The 2-year OS rates for the two groups were 68.0% and 60.8%, respectively.
Regarding safety, neutropenia was the most common adverse event in both the CHOPX and CHOP groups (82% in the CHOPX group and 73% in the CHOP group). The most common grade 3-4 hematologic adverse event in both groups was neutropenia, and the most common grade 3-4 non-hematologic adverse event was infection. In the CHOPX group, 65% (31 patients) reported neutropenia, but no patients experienced prolonged neutropenia (>14 days) or required dose adjustments of the targeted drugs, and 10% (5 patients) experienced infections. In the CHOP group, these proportions were 52% (25 patients) and 4% (2 patients), respectively.
In conclusion, the study results indicate that different targeted drugs combined with CHOP demonstrate good efficacy and safety. These findings provide preliminary evidence supporting the use of CHOPX as a first-line treatment for PTCL patients with different genetic mutations, and suggest that biomarker-driven treatment strategies are feasible and worth further exploration in the future.

 To assess whether the condition is suitable for CAR-T or clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
To assess whether the condition is suitable for CAR-T or clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
WhatsApp: +8613717959070
Email: doctor.huang@globecancer.com
#CancerResearch #LymphomaTreatment #PTCL #TargetedTherapy #Chemotherapy #MedicalBreakthrough #Oncology #ClinicalTrials #ChineseMedicine #CancerSurvivorship #HealthcareInnovation #PrecisionMedicine #CancerTreatment #MedicalResearch #CHOPTherapy #OncologyUpdates #CancerCare
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

**2024 EHA | Breaking Through Multiple Myeloma Treatment Bottlenecks: Significant Advances of Equecabtagene Autoleucel in High-Risk NDMM Patients**
**2024 EHA | Breaking Through Multiple Myeloma Treatment Bottlenecks: Significant Advances of Equecabtagene Autoleucel in High-Risk NDMM Patients**

Multiple Myeloma
Multiple Myeloma (MM) is a malignant plasma cell disorder and one of the most common hematologic malignancies. In China, approximately 20,000 new cases of newly diagnosed multiple myeloma (NDMM) are reported annually, with a median age at diagnosis over 60 years. It is reported that Chinese MM patients generally exhibit higher rates of cytogenetic abnormalities, with an incidence rate exceeding 40%, which is significantly higher than in Western countries.
High-risk MM patients often respond poorly to existing treatment regimens and face limited treatment options. Many elderly patients are frail and have multiple comorbidities, making them less tolerant of the adverse reactions associated with current therapies, particularly autologous stem cell transplantation (ASCT). Once the disease progresses to a refractory/relapsed state, the combination of advanced age, frailty, and high-risk cytogenetic abnormalities leads to limited salvage treatment options, worsening efficacy, and poor prognosis. Thus, selecting effective frontline therapy for NDMM patients, especially high-risk elderly patients unsuitable for transplantation, is a pressing clinical need, requiring innovative therapies to supplement existing treatments. The new generation of cell immunotherapies, exemplified by Equecabtagene Autoleucel, holds promise to fill this gap and potentially become a breakthrough for high-risk NDMM.
In the FUMANBA-1 study, which included 69.5% high-risk patients, Equecabtagene Autoleucel achieved an ORR of 96.1% and has been approved in China for treating third-line or later relapsed/refractory multiple myeloma (R/R MM) patients. This EHA meeting is the first to present oral data on the efficacy and safety of Equecabtagene Autoleucel in the FUMANBA-2 study for high-risk, newly diagnosed, transplant-ineligible MM patients.
### Study Introduction
FUMANBA-2 is a multicenter, open-label, single-arm Phase I study designed to evaluate the efficacy and safety of Equecabtagene Autoleucel in transplant-ineligible NDMM patients with 100% high-risk features (defined by mSMART 3.0: RISS Stage III, double-hit, or triple-hit). Patients received four cycles of induction therapy, including the VRd regimen (Bortezomib, Lenalidomide, Dexamethasone), the VCD regimen (Bortezomib, Cyclophosphamide, Dexamethasone), or the PAD regimen (Bortezomib, Doxorubicin, Dexamethasone). After the third cycle of induction therapy, T cells were collected from patients unsuitable for ASCT and Equecabtagene Autoleucel was prepared. After lymphodepletion, patients received a single infusion of Equecabtagene Autoleucel at a dose of 1.0 x 10^6 CAR-T cells/kg. The primary efficacy endpoints were the proportion of MRD-negative patients and progression-free survival (PFS). Secondary endpoints included objective response rate, duration of response, safety, pharmacokinetics, and pharmacodynamics.
### Study Results
As of January 25, 2024, 16 patients received Equecabtagene Autoleucel, with a median age of 58.5 years (51-69) and a median follow-up time of 13.1 months (7.9-24.3). All patients had high-risk cytogenetics, with 62.5% (10/16) being double-hit, 12.5% (2/16) being triple-hit, and 25% (4/16) having extramedullary disease. 37.5% (6/16) were R-ISS Stage III, with one patient each combining R-ISS Stage III with double-hit and triple-hit characteristics.
The median follow-up time after Equecabtagene Autoleucel infusion was 7.46 months (2.8-18.1). The median PFS was not reached, with a 12-month PFS rate of 84.4% (95% CI: 49.31-96.00). All subjects achieved MRD negativity, with 71.4% (95% CI: 25.8-92.0) maintaining MRD negativity for over 12 months. The objective response rate (ORR) was 100%, with 93.8% (15/16) achieving stringent complete response (sCR).
Grade 1-2 cytokine release syndrome (CRS) occurred in 68.8% (11/16) of patients, with no grade 3 or higher CRS, immune effector cell-associated neurotoxicity syndrome (ICANS), or neurotoxicity. The most common grade 3 or higher drug-related adverse events were hematologic, with a 25.0% (4/16) incidence of grade 3 or higher infectious disease adverse events.
The median peak CAR copy number in peripheral blood was reached on day 10 (7-21) post-infusion, with a median peak level of 79,681.299 copies/μg gDNA. 81.25% (13/16) of patients achieved free B cell maturation antigen (sBCMA) clearance within one month post-infusion. Median peak levels of inflammatory cytokines IL-6, CRP, and ferritin were 64.28 pg/mL (9.12-3017.83), 49.30 mg/L (3.66-117.30), and 553.35 ng/mL (68.10-2349.00), respectively. The median peak times for IL-6 and CRP were day 7 and day 10, respectively, with no significant change in serum ferritin levels compared to pre-infusion.
### Study Outlook
The FUMANBA-2 study of Equecabtagene Autoleucel demonstrates the efficacy and safety of a novel fully human BCMA CAR-T therapy in high-risk, transplant-ineligible, newly diagnosed multiple myeloma patients. This is the first international report of CAR-T therapy as frontline treatment in this specific population. The study highlights the potential application of cell immunotherapy in the MM field. Compared to traditional chemotherapy and new drug treatments, frontline CAR-T therapy for NDMM has the potential to further improve response rates, extend survival, and improve prognosis, particularly for high-risk cytogenetic abnormalities and high tumor burden. For elderly and frail patients who are unsuitable for hematopoietic stem cell transplantation, CAR-T therapy may fill the treatment gap to some extent. The one-time treatment approach, as opposed to continuous chemotherapy or multiple transplants, offers patients better quality of life and treatment convenience. Although CAR-T therapy carries risks such as CRS and neurotoxicity, these side effects are manageable in many studies, and safety improves with treatment experience and management strategies. Bringing CAR-T therapy to the frontline provides patients with more diverse and promising treatment options. However, large-scale, long-term follow-up studies are needed to validate its long-term efficacy and survival benefits, and further exploration and optimization are required for the best administration timing, regimen, and duration.
In summary, the FUMANBA-2 study of Equecabtagene Autoleucel shows significant treatment potential in newly diagnosed, transplant-ineligible multiple myeloma patients. With accumulating research evidence and advances in CAR-T technology, we anticipate CAR-T therapy will benefit more patients in the future.
🎉🎉To assess whether the condition is suitable for CAR-T or clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
WhatsApp: +8613717959070
Email: doctor.huang@globecancer.com
#EquecabtageneAutoleucel #MultipleMyeloma #MMTreatment #HighRiskMM #NDMM #CAR_Therapy #Immunotherapy #BloodCancer #OncologyResearch #EHA2024 #CancerBreakthrough #CellTherapy #MyelomaTreatment #ClinicalTrials #InnovativeMedicine #HealthcareAdvancements
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Putin Says Russia Is Close to Creating Cancer Vaccines. A Look at China’s Advancements
Putin Says Russia Is Close to Creating Cancer Vaccines. A Look at China’s Advancements

Putin
Recently, a viral piece of information has swept the internet. According to reports, Russian President Putin revealed that Russian scientists are close to developing a cancer vaccine and a new generation of immunomodulatory drugs, which can soon be made available to patients for effective personalized treatment.
However, Putin did not specify which type of cancer this vaccine would prevent or how it would prevent it. Nevertheless, this news has spread widely internationally, with some even exaggerating its effectiveness. So, is this really true?
It is reported that the information revealed by President Putin is indeed true and will soon be used for personalized treatment. It can be confirmed that this cancer vaccine is a therapeutic vaccine. However, it is not a treatment for all types of cancer but rather a “highly customized” vaccine based on a certain gene sequencing, targeting different mutation sites, including multiple sites, for each patient.
Cancer vaccines are a form of active immunotherapy and an important part of tumor immunotherapy. They work by stimulating or restoring the body’s own immune system to prevent cancer development or kill existing tumors. Cancer vaccines mainly include cell vaccines, DNA vaccines, mRNA vaccines, peptide vaccines, dendritic cell vaccines, nano vaccines, etc., and have shown promising clinical efficacy in the treatment of solid tumors such as malignant melanoma, lung cancer, ovarian cancer, and cervical cancer.

Cancer Vaccines
According to data from clinicaltrials.gov, China has about 150 ongoing tumor vaccine projects. China’s first mRNA tumor vaccine is targeting FDA approval, and more tumor mRNA vaccines are emerging, targeting lung cancer, pancreatic cancer, breast cancer, and more.
The personalized tumor neoantigen vaccine LK101 injection has been approved for clinical use!
On March 15, 2023, according to the official website of the National Medical Products Administration Drug Evaluation Center (CDE), the new drug clinical trial application (IND) of the personalized tumor neoantigen vaccine “LK101 injection” independently developed by Beijing Likang Life was approved for the treatment of advanced solid tumors.
It is reported that this product is the first domestically approved personalized tumor neoantigen vaccine to enter clinical stage and the first completely personalized mRNA editing product approved for clinical stage in China, marking a milestone event in the field of mRNA tumor vaccines in China.
On December 22, 2022, LK101 injection submitted a new drug clinical research application (IND) and was accepted. This personalized tumor neoantigen vaccine adopts the form of mRNA-DC (mRNA-dendritic cell) vaccine, which transfects dendritic cells with mRNA encoding tumor neoantigens ex vivo. The vaccine not only has high safety and good tolerance but also can provide patients with long-term anticancer effects.
Disease iNeo-Vac-P01 new antigen vaccine!
Personalized cancer vaccines significantly effective against a wide range of advanced solid tumors
The research team of Zhejiang Shao Yifu Hospital designed a peptide-based neoantigen vaccine iNeo-Vac-P01 and conducted a prospective clinical trial, enrolling a total of 22 patients with standard treatment failure and a wide range of advanced solid tumors. Using the iNeo artificial intelligence vaccine design platform, personalized peptide drug preparation and quality control system were used to customize iNeo-Vac-P01 vaccine for each patient.
After treatment, the results showed that among the 22 patients with advanced malignant tumors, 20 had no adverse reactions or had mild adverse reactions. The disease control rate was 71.4%, and the median progression-free survival was 4.6 months, with the median survival not yet reached.
The study suggests that for patients with advanced solid tumors, iNeo-Vac-P01 monotherapy is feasible and safe. It can induce T-cell-mediated immune responses against tumor neoantigens and may have good anti-tumor efficacy.
JCXH-211: Targeting multiple solid tumors with tumor neoantigen mRNA vaccine
Recently, a tumor neoantigen mRNA vaccine developed by Jiachen Xihai Biotechnology Co., Ltd. JCXH-211 has obtained FDA’s IND approval. JCXH-211 is a novel drug based on self-replicating mRNA encoding interleukin-12 (IL-12), which can express IL-12 in the body at a low dose for a long time and is suitable for the potential treatment of various advanced solid tumors.
Preclinical studies have shown that JCXH-211 can effectively kill tumor cells, eliminate distant tumors, and prevent tumor recurrence. This excellent tumor clearance effect is due to the strong antiviral immune response induced by RNA replicons and the strong antitumor immune response activated by IL-12. In comprehensive GLP toxicological studies, JCXH-211 has shown high safety.
The Phase 1 clinical trial of JCXH-211 will evaluate the efficacy of single-agent JCXH-211 in patients with advanced malignant solid tumors who have progressed or cannot tolerate existing treatments after receiving current treatment. This trial is open to patients aged 18 or older with at least one tumor lesion suitable for IT injection, measurable disease according to RECIST1.1, sufficient organ function, and an ECOG physical status of 0 to 1. Let’s wait and see its effectiveness!
#JCXH211 #cancer #CancerVaccine #ImmunotherapyBreakthrough #PersonalizedTreatment #TumorVaccine #mRNAVaccine #NeoantigenVaccine #CancerResearch #PrecisionMedicine #ClinicalTrials #MedicalInnovation
