Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Blood Cancer – Diagnosis and Treatment Tips
 Blood Cancer – Diagnosis and Treatment Tips
Blood Cancer – Diagnosis and Treatment Tips 

Blood Cancer
Blood cancer, encompassing types such as leukemia, lymphoma, and multiple myeloma, represents a significant health challenge in regions like Southeast Asia and India. These hematologic malignancies arise from blood-forming cells and can impact the bone marrow, blood, and various organs. The increasing prevalence of these diseases is concerning, yet advancements in diagnosis and treatment provide hope for patients.
## Understanding Hematologic Malignancies
 Hematologic malignancies include a variety of cancers such as:
Hematologic malignancies include a variety of cancers such as:
– **Leukemia**: Cancer of the bone marrow that leads to the overproduction of abnormal white blood cells.
– **Lymphoma**: Affects the lymphatic system and includes #Hodgkin and #nonHodgkinlymphoma.
– **Multiple Myeloma**: Cancer that forms in plasma cells, affecting the production of antibodies.
 The causes of these conditions are multifactorial, involving genetic factors, immune dysfunction, exposure to environmental toxins, and lifestyle choices. For instance, a diet high in processed foods, sedentary behavior, and high stress levels can contribute to an increased risk of developing these cancers.
The causes of these conditions are multifactorial, involving genetic factors, immune dysfunction, exposure to environmental toxins, and lifestyle choices. For instance, a diet high in processed foods, sedentary behavior, and high stress levels can contribute to an increased risk of developing these cancers.
## The Rising Incidence of Blood Cancer
The incidence of blood cancers is on the rise globally, particularly in countries with aging populations. In Southeast Asia and India, there has been a noticeable increase in cases of leukemia and lymphoma, necessitating better awareness and improved healthcare infrastructure.
## Diagnosis: Early Detection is Key
Early diagnosis is crucial for successful treatment outcomes. Patients experiencing symptoms such as unexplained fatigue, frequent infections, easy bruising, or swollen lymph nodes should seek medical advice promptly. Healthcare providers may utilize blood tests, bone marrow biopsies, and imaging studies to diagnose these conditions accurately.
## Treatment Advances: A Diverse Approach
Recent years have seen significant advancements in the treatment of hematologic malignancies, offering patients more options than ever before:
1. **Combination Chemotherapy**: Despite potential side effects, combination chemotherapy remains a cornerstone treatment. New regimens are being developed that combine traditional cytotoxic drugs with targeted therapies and immunotherapies to enhance efficacy and reduce toxicity.
2. **Targeted Therapies**: Drugs that specifically target cancer cell mutations or characteristics are revolutionizing treatment. For example, *Gleevec*, the first targeted therapy, has dramatically improved survival rates for chronic myeloid leukemia (#CML).
3. **Monoclonal Antibodies**: Often dubbed “biological missiles,” these treatments target specific proteins on cancer cells, allowing for more precise treatment with fewer side effects.
4. **Hematopoietic Stem Cell Transplantation**: This procedure remains one of the most effective treatments for certain types of blood cancer, especially when other treatments fail.
5. **Immunotherapy**: This approach harnesses the body’s immune system to fight cancer. Techniques like CAR-T cell therapy, which modifies a patient’s T cells to attack cancer cells, have shown promising results in treating various hematologic malignancies. China is at the forefront of CAR-T cell therapy research and application, particularly in treating hematologic malignancies. CAR-T therapy involves extracting a patient’s T cells, modifying them to specifically recognize and attack cancer cells. Clinical research and applications in China have shown remarkable effectiveness in treating leukemia, lymphomas, and multiple myeloma. Some studies indicate that patients receiving CAR-T treatment experience significantly higher long-term survival rates and lower recurrence rates. Furthermore, China has made significant progress in the standardization of CAR-T therapy, personalized treatment plans, and the development of technological platforms, enabling more patients to benefit from this innovative treatment.
## Hope for the Future
Countries like India and those in Southeast Asia are rapidly advancing in the field of blood cancer treatment. Collaborative efforts among healthcare professionals, research institutions, and patient advocacy groups are crucial for improving access to cutting-edge therapies. The development of treatment guidelines tailored to the regional context can ensure that patients receive the best possible care.
### Conclusion
Hematologic malignancies are challenging but treatable diseases. Through early diagnosis and the application of innovative therapies, patients can achieve significant improvements in their health and quality of life. As research continues to evolve, the prospect of long-term survival and even cures for blood cancers is becoming increasingly attainable. Empowering patients with knowledge and access to modern treatments is essential to fighting blood cancer effectively in #SoutheastAsia and #India.

 To assess whether the condition is suitable for clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
To assess whether the condition is suitable for clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
WhatsApp: +8613717959070
Email: doctor.huang@globecancer.com
#HematologicMalignancies #LeukemiaAwareness #LymphomaResearch #MultipleMyeloma #BloodCancer #CancerResearch #CAR_Therapy #StemCellTransplant #Immunotherapy #TargetedTherapy #MonoclonalAntibodies #CancerTreatment #MedicalAdvancements #CancerSurvivor #HealthcareInnovation #ALL #AML
The Emergence of Fifth Generation CAR-T: A Boon for Late-Stage Cancer Patients or a Major Breakthrough in Solid Tumor Treatment?
The fifth-generation CAR-T is designed as a universal type of CAR-T. Is this risk-free CAR-T capable of achieving significant breakthroughs in solid tumor treatment, or is it effectively reducing costs to enable scalable production and treatment?
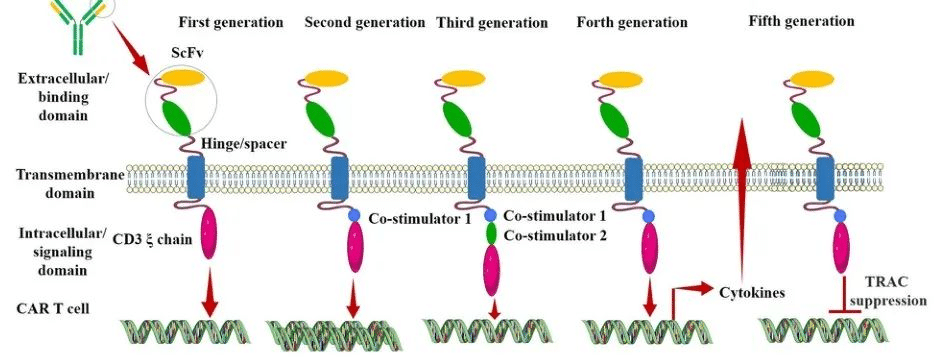
After nearly three decades of development, CAR (Chimeric Antigen Receptor) technology has undergone continuous innovation. Currently, CAR has evolved to its fifth generation. Its aim is to enhance the safety of treatments by reducing toxicity and non-specific antigen recognition. This is achieved by stimulating proliferation, activation, and the generation of memory phenotypes within CAR-T cells to improve efficiency and provide immune regulation for the optimal function of CAR-T cells.
Generation CAR-T
The Evolution of Different Generations of CAR-T
First Generation CAR:
The first-generation CAR comprises an extracellular single-chain variable fragment (scFv) as the antigen recognition binding domain and an intracellular CD3ζ as the cellular activation signaling domain. Despite initiating cytotoxic anti-tumor responses within transplanted T cells, first-generation CAR-T cells exhibit lower levels of cytotoxicity and proliferation due to the CAR structure lacking co-stimulatory domains, which results in inadequate interleukin (IL)-2 production.
Second Generation CAR:
Building upon the CD3ζ signal transduction domain, the second-generation CAR includes an additional co-stimulatory signaling domain that activates T cells, significantly enhancing T cell proliferation and survival. For instance, CD28 can deliver robust activation signals, enabling T cells to achieve high levels of cytotoxic activity in a shorter duration, while 4-1BB provides prolonged activation signals, sustaining T cell-mediated killing of tumor cells. However, limitations arise in second-generation CAR-T cells utilizing retroviruses as viral vectors, restricting the length of transgene fragments they can carry. As a result, it becomes necessary to choose between incorporating CD28 and 4-1BB into T lymphocytes.
Third Generation CAR:
Third-generation CAR-T cells utilize larger DNA-carrying lentiviruses as viral vectors, allowing simultaneous incorporation of DNA fragments for both CD28 and 4-1BB into T cells. Consequently, the third-generation CAR structure encompasses two co-stimulatory domains, theoretically addressing the need for higher activation intensity and sustained survival of CAR-T cells. However, the safety concerns associated with prolonged and high-level persistence of CAR-T cells, including potential attacks on the host’s immune system, remain unresolved despite these advancements.
Fourth Generation CAR:
The design concept behind the fourth-generation CAR revolves around the precise treatment of cancerous diseases. For instance, solid tumors generate a microenvironment (TME) during their chronic progression, preventing CAR-T cells from penetrating the tumor interior. As a result, CAR-T therapy demonstrates limited efficacy in treating solid tumors. TRUCK CAR-T involves incorporating cytokines (such as IL-12) or chemokines into the CAR structure. This facilitates increased infiltration of T cells into tumor tissues while recruiting other immune cells within the body to eliminate tumor cells. In some studies, a suicide gene or certain drug-sensitive genes are attached to the CAR structure to ensure the clearance of CAR-T cells from the body post-treatment, preventing inadvertent harm to normal cells and enhancing the safety and controllability of CAR-T therapy.
Fifth Generation CAR:
The fifth-generation CAR-T, known as universal CAR-T, achieves T-cell receptor α (TCR-α) and β (TCR-β) chain deletion by knocking out the TRAC gene. This implies the removal of the T-cell receptor (TCR) from the surface of T cells, thereby avoiding the occurrence of graft-versus-host disease (GVHD) in transplantation reactions.
Since the FDA’s approval of the CD19 CAR-T product, Novartis’s Kymriah, in 2017, CAR-T cell therapy has entered a stage of rapid development. However, the currently approved and marketed products are all second-generation CAR-T therapies. There is still a long way to go for CAR-T to become widespread in the market.
Safety concerns constitute the primary challenge for CAR-T, such as off-target effects, cytokine release syndrome (CRS), and neurotoxicity (NTX). Currently available CAR-T products primarily focus on treating hematologic malignancies, with no major breakthroughs achieved yet in treating solid tumors.
In 2021, China’s NMPA approved three CAR-T products for marketing: FOSUNKITE’s Axicabtagene Ciloleucel injection, JW Therapeutics’s Relmacabtagene Autoleucel Injection, and the recently approved JUVENTAS’s Inaticabtagene Autoleucel Injection, all targeting CD19. Additionally, earlier this year, IASO Bio obtained approval for Equecabtagene Autoleucel Injection, targeting BCMA. While CAR-T targeting CD19 has shown effectiveness, its scope remains limited to B-cell-related hematologic malignancies. BCMA-targeted CAR-T is restricted to treating multiple myeloma. To address solid tumor treatment, the development of more specific and potent targets is necessary.
Among the recently released domestically developed JUVENTAS’s Inaticabtagene Autoleucel Injection, its competitive advantage lies in its price, which has decreased to below one million RMB(Approximately $140,000 US).
With the continuous advancement of molecular biology technologies, more breakthroughs are expected in CAR molecule design. This progression anticipates the development of safer and more efficient universal CAR-T therapies in the future, benefiting a broader spectrum of cancer patients.
“If you’d like to inquire about the latest cancer-fighting technologies and treatments, you can contact us.”
whatsapp:+8613717959070
#CARTCellTherapy #CancerTreatment #ScienceInnovation #GeneticMedicine #TumorTreatment #HealthcareTech #MedicalScience #CancerAwareness #PatientCare #FutureOfMedicine
