Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79
New Advances in Chinese CAR-T Cell Therapy: CD27 Armored BCMA CAR-T Shows Potential in Treating Relapsed Multiple Myeloma
**New Advances in Chinese CAR-T Cell Therapy: CD27 Armored BCMA CAR-T Shows Potential in Treating Relapsed Multiple Myeloma**
Multiple Myeloma
#BCMA #CD27#CARTCellTherapy #RRMM #MM #MultipleMyeloma #CART
Relapsed and refractory multiple myeloma (RRMM) is a challenging blood cancer that poses significant obstacles for patients. Although several BCMA (B-cell maturation antigen) targeting CAR-T cell therapies have been developed, achieving long-term remission and extended survival remains difficult. The recent introduction of CD27-armored BCMA CAR-T—CBG-002—by a Chinese medical team brings new hope for RRMM patients. Based on preclinical data, this therapy shows promising anti-myeloma activity, with Phase I clinical trial results further validating its efficacy and safety.
Research Highlights
CBG-002 is an innovative therapy that enhances traditional BCMA CAR-T by adding a CD27 costimulatory domain. The inclusion of CD27 improves CAR-T cell persistence and activity, contributing to stronger anti-cancer effects. Recently published Phase I research in Cancer Immunology Research indicates that this CD27-armored BCMA CAR-T therapy is not only well-tolerated but also shows notable efficacy in RRMM patients.
The study enrolled 11 RRMM patients, all of whom had undergone three or more prior treatments, with a median age of 54. The results showed that 81.8% of patients experienced only mild cytokine release syndrome (CRS) and no severe neurotoxicity. Even at a low dosage level (1-3×10^6 CAR-T cells/kg), CBG-002 achieved a high overall response rate (ORR) of 81.8%, with 45.5% of patients reaching stringent complete remission.
Future Outlook
The Phase I study of CBG-002 not only confirmed its efficacy but also demonstrated advantages in production time and cost. Compared to current products on the market, CBG-002 has a shortened production cycle of just 10 days, making it a timely and affordable treatment option for more patients. Amid global progress in CAR-T cell therapies, the innovation by this Chinese medical team positions it as a significant force in advancing cancer research worldwide.
🎉🎉To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of <Advanced Medicine in China> for preliminary evaluation!
WhatsApp: Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#MultipleMyeloma #CancerResearch #Immunotherapy #ChinaBiotech #Oncology
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

CAR-T Cell Therapy as a New Option for Treating Multiple Myeloma
**CAR-T Cell Therapy as a New Option for Treating Multiple Myeloma**

Multiple Myeloma
“CAR-T cell therapy has now become a new option for treating patients with relapsed and refractory multiple myeloma, with hopes of changing the difficult situation in myeloma treatment where treatments are either ineffective or unavailable,” said Jin Jie, Director of the Hematology Department at the First Affiliated Hospital of Zhejiang University School of Medicine, in an interview with People’s Daily Health on October 23.
Early on October 23, Jin Jie visited the hospital ward to see a 72-year-old patient with multiple myeloma. Just the day before, the patient had begun receiving treatment with a domestically produced BCMA-targeting CAR-T drug.
“This 72-year-old patient came to the hospital due to bone pain and was even unable to walk steadily,” Jin recalled. After being diagnosed with multiple myeloma, the patient initially received a series of chemotherapy regimens that showed some efficacy. However, a year after undergoing autologous hematopoietic stem cell transplantation, the disease relapsed, and various subsequent treatments proved suboptimal. As a result, the patient opted for CAR-T therapy.
Since the approval of Equecabtagene Autoleucel last year, Professor Jin Jie became one of the first doctors nationwide to prescribe CAR-T drugs for multiple myeloma. This patient is her tenth multiple myeloma patient to receive this innovative therapy. Discussing the treatment outcomes, Jin noted, “The overall efficacy for patients has been very good.” A month ago, another patient who underwent this CAR-T therapy returned for a follow-up. “Everything was going well; we will continue to monitor the patient’s indicators until all data are stable.”
Multiple myeloma is a malignant plasma cell disease that predominantly affects older adults. Jin observed that the incidence of multiple myeloma has been trending younger in recent years, with patients in their forties commonly seen in clinical settings. Currently, multiple myeloma remains an incurable disease, and most patients face inevitable relapse. However, thanks to the emergence of new drugs and advances in treatment, both the efficacy and overall survival of patients have significantly improved in recent years.
“CAR-T therapy involves collecting a patient’s T cells and equipping them with a ‘weapon.’ These T cells are then expanded outside the body and re-infused into the patient, where they target and attack tumor cells, while also being able to proliferate in the patient’s body to eliminate cancer cells,” Jin explained. CAR-T therapy has the potential to give patients a higher quality of life.
CAR-T cell therapy has been advancing rapidly in the field of multiple myeloma, with multiple products already approved and available. In Jin’s view, patients should, under professional guidance, choose drugs and treatments with extensive clinical experience and proven efficacy.
🎉🎉To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of <Advanced Medicine in China> for preliminary evaluation!
WhatsApp: Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
**#MultipleMyeloma #CAR_TCellTherapy #CancerTreatment #Immunotherapy #Hematology #CellTherapy #MedicalInnovation #PatientCare #Oncology #ZhejiangUniversity**
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

China’s CAR-T Therapy: A Beacon of Hope for Children with Acute Lymphoblastic Leukemia (ALL)
China’s CAR-T Therapy: A Beacon of Hope for Children with Acute Lymphoblastic Leukemia (ALL)

#CARTTherapy #Leukemia #ChildhoodCancer #ALL #CART #AcuteLymphoblasticLeukemia #Patientstory
China’s CAR-T cell therapy is emerging as a beacon of hope in the fight against cancer, bringing unprecedented treatment possibilities. As a precise cellular immunotherapy, CAR-T therapy enhances the cancer-fighting abilities of T-cells through genetic editing technology, offering breakthroughs for patients with cancers resistant to traditional treatments, especially in blood cancers like leukemia.
From Diagnosis to Treatment: Strength and Struggle
Shan is a young child in China who has endured long-term treatment for leukemia. Diagnosed with acute lymphoblastic leukemia (ALL) in 2019, this news brought immense suffering to her and her family, as she was only five years old. Although ALL generally responds well to chemotherapy, Shan’s cancer cells persisted stubbornly after several rounds of chemotherapy, failing to reach full remission. Her doctors recommended a bone marrow transplant, but due to physical and family constraints, she had to opt for conservative treatment. Nevertheless, Shan did not give up her desire to live, showing remarkable resilience over five years.
A New Hope Through CAR-T Therapy
In 2023, Shan’s condition worsened as her anemia grew severe, with her hemoglobin levels dropping to a critical point. Faced with despair, her mother reached out to our team at Advanced Medicine in China, where experts quickly admitted her to the hospital. After a comprehensive evaluation, our hematology-oncology specialists decided to proceed with CAR-T therapy for her.
Following a thorough process of gene modification and the infusion of CAR-T cells, Shan’s condition improved rapidly. In the early stages of treatment, her complexion brightened, her energy levels noticeably improved, and subsequent tests showed that her tumor cells had completely disappeared, achieving clinical remission. Shan was finally free from the shadow of cancer, gradually regaining the joy and health of childhood.
A Medical Breakthrough: New Hope for Children with Leukemia
Shan’s success story signifies the maturation of CAR-T therapy in China, showcasing its powerful potential, particularly in treating refractory and relapsed childhood acute leukemia. In recent years, Chinese medical teams have actively adopted CAR-T technology in treating pediatric blood cancers, achieving remarkable long-term remission for many children. As the country with the highest number of CAR-T therapy applications globally, China’s hospital teams possess extensive experience and advanced technological capabilities, offering high-quality treatment to more children suffering from relapsed and refractory blood diseases.
Moving Forward: A Promising Future for Cellular Immunotherapy
With the continued development of CAR-T therapy in China, more patients with challenging cancers stand to benefit. Shan’s recovery is not only a family’s joy but also a testament to China’s medical progress. CAR-T therapy is ushering in a new era of cellular immunotherapy, giving more patients the possibility of life extension and recovery.
🎉🎉To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of <Advanced Medicine in China> for preliminary evaluation!
WhatsApp: Https://wa.me/+861371795907
Email: doctor.huang@globecancer.com
#CancerResearch #MedicalBreakthrough #Immunotherapy #ChinaMedicine #Oncology #CancerHope #LeukemiaAwareness #CancerTreatment
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

China’s CAR-T Therapy as a Beacon of Hope: A New Light for Multiple Myeloma Patients
**China’s CAR-T Therapy as a Beacon of Hope: A New Light for Multiple Myeloma Patients**

Multiple Myeloma
#CAR-TTherapy #MultipleMyeloma #PatientStory #CancerSurvivor
In recent years, CAR-T cell therapy in China has spearheaded a revolution in hematologic cancer treatment. This innovative immunotherapy has brought a glimmer of hope to many patients, especially those with relapsed and refractory cases who have exhausted traditional treatments. We recently interviewed Ms. Chen, a 53-year-old multiple myeloma patient who reached complete remission (CR) following CAR-T therapy, in hopes that her journey will inspire confidence and encouragement in other patients facing similar challenges.
**Ms. Chen’s Treatment Journey**
Ms. Chen, once a restaurant owner, was misdiagnosed with lumbar spondylolisthesis in 2019 due to chronic back pain and underwent surgery. However, her symptoms worsened post-surgery, and she was ultimately diagnosed with multiple myeloma with high-risk cytogenetic features. The sudden diagnosis was devastating, and she considered abandoning treatment. Encouraged by her family and reassured by her doctors, she decided to face the disease head-on and began treatment.
After multiple rounds of chemotherapy, Ms. Chen saw some improvement, but her condition continued to relapse. As her condition worsened and traditional therapies proved ineffective, she reached out to our Advanced Medicine in China team. After an expert consultation, Ms. Chen was offered the chance to receive CAR-T therapy, and with the support of her family and medical team, she found renewed hope.
**The Miracle of CAR-T Therapy**
A few days after her cells were collected and reinfused, Ms. Chen experienced side effects such as fever and headache. With close monitoring by our expert team, her side effects gradually came under control. After completing CAR-T therapy, her condition was effectively managed, allowing her to return to a normal lifestyle. Today, she can handle household chores and has gradually returned to work, leading a healthy and fulfilling life.
**Ms. Chen’s Advice and Encouragement**
-
**Trust Science and Doctors**: Persist with treatment and believe in the power of science—don’t give up easily.
-
**Maintain Good Communication**: Work closely with your doctors and trust their expertise.
-
**Stay Positive**: Approach the illness with positivity, avoiding anxiety and fear.
-
**Focus on Nutrition**: Ms. Chen believes dietary supplementation is better than medication and boosts immunity through balanced nutrition.
-
**Embrace a Healthy Lifestyle**: She often walks in the park, enjoys sunlight, and cherishes a restored, healthy life.
**Expert Opinion: The Advantages and Prospects of China’s CAR-T Therapy**
CAR-T therapy has become a groundbreaking treatment option due to its high specificity for hematologic malignancies. Compared with traditional therapies, China’s CAR-T therapy offers distinct advantages:
-
**High Specificity**: Chinese CAR-T cells can precisely identify and destroy cancer cells, reducing harm to normal tissues.
-
**Short Treatment Cycle**: Unlike conventional multi-round treatments, China’s CAR-T therapy typically requires only one infusion, with fewer side effects.
-
**Deep and Durable Responses**: Chinese CAR-T cells can survive in the body long-term and continually eliminate cancer cells.
Data shows that the overall survival rate for multiple myeloma patients treated with CAR-T is 92.9% over three years, highlighting its tremendous potential in enhancing both patient quality of life and longevity.
**Conclusion**
China’s CAR-T therapy brings new hope to patients with relapsed and refractory hematologic malignancies, and cases like Ms. Chen’s are on the rise. We hope her story will offer strength and confidence to patients currently battling illness.
🎉🎉To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of <Advanced Medicine in China> for preliminary evaluation!
WhatsApp: Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#CancerTreatment #MedicalBreakthrough #ChinaMedicalAdvances #Immunotherapy #HealthcareInnovation #HopeAndHealing #AdvancedMedicine
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

China’s CSPC Pharmaceutical Group CAR-T Therapy: Targeted Treatment for Myasthenia Gravis
China’s CSPC Pharmaceutical Group CAR-T Therapy: Targeted Treatment for Myasthenia Gravis

Myasthenia Gravis
#CARTTherapy #MyastheniaGravis #ChinaPharma #CSPC #CART
China’s CAR-T cell therapies are attracting international attention. Recently, CSPC Pharmaceutical Group secured another clinical trial approval for a CAR-T therapy, marking a significant milestone in the treatment of autoimmune diseases. China’s National Medical Products Administration (NMPA) Center for Drug Evaluation (CDE) officially approved CSPC’s innovative therapy, SYS6020-CAR-T cell injection, for the treatment of refractory generalized myasthenia gravis. This advancement offers new hope for patients with neuromuscular autoimmune diseases.
Chinese Innovation: An mRNA-LNP-Driven CAR-T Product
SYS6020 is a chimeric antigen receptor (CAR-T) cell injection based on mRNA-LNP technology, representing CSPC Pharmaceutical’s first innovation in cell therapy. It is designed to precisely target BCMA-positive B cells and plasma cells, thereby blocking harmful antibody production, significantly alleviating symptoms, and improving patients’ quality of life. Previously, this product had obtained clinical trial approval for systemic lupus erythematosus, and this recent approval marks another successful expansion into the autoimmune disease field.
New Hope for Myasthenia Gravis Treatment: Addressing Long-Term Relapse Issues
Myasthenia gravis is an autoimmune neuromuscular disease caused by autoantibodies, leading to neuromuscular transmission impairment. Some patients struggle with inadequate control under existing treatments, facing recurring relapses and a need for hospitalization. By selectively depleting BCMA-positive cells, SYS6020 aims to achieve long-term symptom improvement and reduce patients’ dependency on immunosuppressants and cholinesterase inhibitors.
CAR-T Therapy in China: More Effective, Safer
SYS6020 demonstrates high cellular activity and CAR-positive rates while significantly reducing risks associated with traditional CAR-T therapies, such as genome integration-related oncogenic risks and cytokine release syndrome (CRS), offering enhanced safety. In June of this year, the therapy received its first clinical approval for relapsed or refractory multiple myeloma, followed by clinical trial approval for systemic lupus erythematosus, laying the foundation for further expansion into myasthenia gravis treatment.
Summary: Future Developments
CSPC Pharmaceutical has stated that the clinical approval of SYS6020 for myasthenia gravis is a landmark achievement in cell therapy. In the future, CSPC will continue advancing SYS6020’s development for oncology, autoimmune connective tissue diseases, and neuromuscular autoimmune diseases, aiming to provide breakthrough treatment options and tangible clinical benefits for more patients. This groundbreaking progress not only drives CAR-T therapy development in China but also brings new treatment hope to autoimmune disease patients worldwide.
🎉🎉To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of <Advanced Medicine in China> for preliminary evaluation!
WhatsApp: Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#CAR-TTherapy #MyastheniaGravis #ChinaPharma #AutoimmuneDisease #NeuromuscularDisorders #mRNALNP #MedicalBreakthrough #Immunotherapy #ClinicalApproval
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79
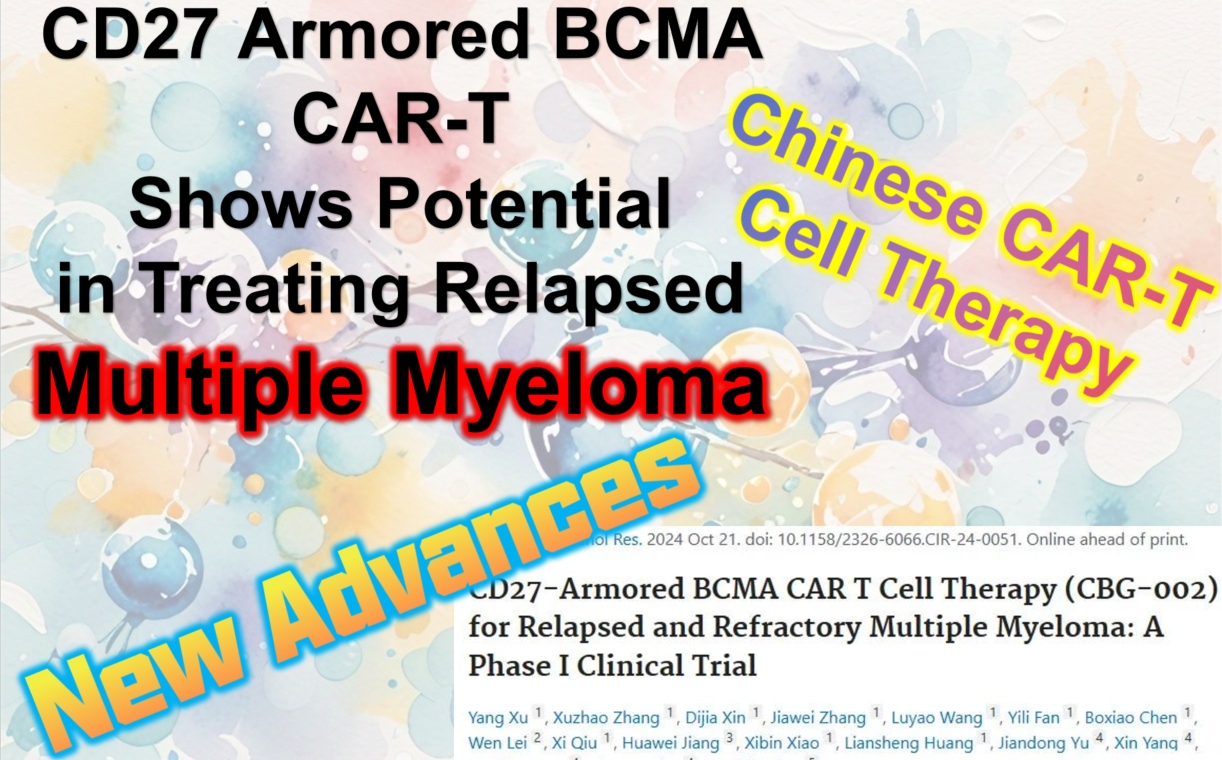
What Kind of Multiple Myeloma Patients Are Suitable for CAR-T Therapy in China?
# What Kind of Multiple Myeloma Patients Are Suitable for CAR-T Therapy in China?
Multiple Myeloma
#MultipleMyeloma #CAR_Therapy #MM #CART #RRMM #Hematology
**Multiple Myeloma** (MM) is a malignant hematological disease that affects plasma cells. In recent years, various drugs and treatment methods, such as proteasome inhibitors, immunomodulatory drugs, and autologous stem cell transplantation, have significantly improved the prognosis of multiple myeloma patients. However, a considerable number of patients still experience relapses and refractory disease. For these patients, CAR-T cell therapy is emerging as a groundbreaking and effective treatment option.
China has made remarkable progress in CAR-T therapy technology in recent years, becoming a global leader in the field of hematological diseases. This has attracted patients worldwide to seek this advanced treatment. So, which multiple myeloma patients are suitable to receive CAR-T treatment in China?
## 1. **Indications: Preferred Choice for Drug-Resistant/Relapsed/Refractory Multiple Myeloma Patients**
CAR-T therapy is typically recommended for multiple myeloma patients who have developed resistance to standard treatments (such as proteasome inhibitors, immunomodulatory drugs, and monoclonal antibodies) and are in their third line of treatment or beyond. In China, CAR-T therapy has broader indications and better efficacy.
### Suitable Patient Types:
-
Relapsed or refractory multiple myeloma patients, typically those who have undergone at least second-line treatments.
-
Patients with high-risk genetic characteristics, such as certain mutations (e.g., 17p deletion, t(4;14) translocation).
-
Patients unable to tolerate traditional treatments, including chemotherapy, other targeted therapies, stem cell transplantation, or immunomodulatory treatments, due to poor tolerance or severe side effects.
-
Patients who are BCMA-positive.
-
Patients whose disease continues to progress despite other treatments, especially chemotherapy.
-
Patients who are ineligible for stem cell transplantation.
-
Patients with severe symptoms not responsive to conventional treatments, such as bone pain, anemia, hypercalcemia, and kidney damage.
-
High tumor burden patients—experts generally reduce the tumor burden first before administering CAR-T therapy, often through bridging or sequential treatments.
Among the four global CAR-T products targeting the BCMA marker in multiple myeloma, two Chinese products stand out for their efficacy and affordability. The most effective product currently is IASO Bio’s FUCASO (Equecabtagene Autoleucel), with a complete response (CR) rate of 82.4%.
## 2. **Patients in Good Physical Condition**
CAR-T therapy is essentially a powerful immunotherapy. Although it has remarkable efficacy, it also carries some risks of side effects, including cytokine release syndrome (CRS) and neurotoxic reactions. China’s CAR-T treatment system is highly developed, with established treatment plans and consensus. The country has extensive experience in managing CRS, neurotoxins, and side effects, keeping the risks very low. Moreover, the expert doctors at Advanced Medicine in China have substantial experience in managing these risks. Nonetheless, patients are typically required to have stable physical health to withstand the risks associated with the treatment.
– Overall good physical function; patients with heart, lung, liver, or kidney dysfunction may require a secondary evaluation by an expert team.
– Patients need to score 0-1 on the ECOG performance status scale, indicating that they are capable of daily activities and self-care.
## 3. **Patients with Financial and Time Support for CAR-T Therapy**
CAR-T therapy’s high cost and complex manufacturing process require patients and their families to have financial support. CAR-T therapy in China is significantly more affordable than in Western countries. While CAR-T treatments in the U.S. may cost $600,000 to $700,000, China’s approved CAR-T treatments cost around $100,000, about one-fifth to one-seventh of U.S. prices. Nevertheless, it remains a high-cost treatment, so patients need to be fully aware of the expenses involved.
China has invested heavily in CAR-T research in recent years. Many top hospitals and research institutions conduct related clinical trials. China accounts for over 50% of global CAR-T clinical trials. If a patient qualifies for a clinical trial, participating in it could be a more economical option, offering access to the latest CAR-T therapies, sometimes costing only tens of thousands of dollars or even free.
The CAR-T treatment process is relatively long. It involves collecting T cells, modifying them, re-injecting them, and close monitoring, requiring the patient to have enough time and patience to complete the entire process. The fastest known case took two weeks to complete all steps and discharge with complete response (CR), but generally, the process takes about four weeks or longer, depending on the patient’s condition.
For patients who can afford the treatment and have the time to complete it, CAR-T therapy in China is undoubtedly an attractive option.
## Conclusion
China’s leading position in CAR-T cell therapy technology and lower treatment costs make it a popular destination for multiple myeloma patients worldwide. It offers new hope for relapsed or refractory multiple myeloma patients. By working with experienced medical teams, patients can receive more personalized treatment plans and benefit from the rapid development of CAR-T therapy globally.
🎉🎉To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of <Advanced Medicine in China> for preliminary evaluation!
WhatsApp: Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#CancerTreatment #ChinaMedicalInnovation #Immunotherapy #MyelomaTreatment #AdvancedMedicine #RelapsedMyeloma #CancerResearch
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

**CAR-T Therapy: A New Hope for Effective Immunotherapy or an Expensive Challenge?**
**CAR-T Therapy: A New Hope for Effective Immunotherapy or an Expensive Challenge?**
As an innovative immunotherapy, CAR-T therapy has gradually become available in China in recent years, attracting significant attention from patients. Although it is dubbed the “million-dollar therapy” due to its high cost, experts emphasize that CAR-T is not a conventional drug but a “living drug.” Its effectiveness is confirmed, but the outcome largely depends on the skill and experience of the operator. Like a horse-riding competition, the handler must fully understand and control this “good horse.” Early data show promising results, and while the overall treatment cost remains high, its efficacy is undeniable.
To assess whether the condition is suitable for clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
WhatsApp: Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#cart #carttherapy #CAR_T #leukemia #lymphoma #cancer #tumor #bloodcancer
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

**The Miracle of CAR-T Therapy in China: Mrs. Li’s Battle Against Lymphoma**
**The Miracle of CAR-T Therapy in China: Mrs. Li’s Battle Against Lymphoma**

patient story
In the long journey of life, cancer often strikes like a sudden storm, leaving patients and their families devastated. Mrs. Li, a young and resilient mother from China, was no exception. Two years ago, she was diagnosed with relapsed and refractory B-cell non-Hodgkin lymphoma. The shocking news felt like a bolt from the blue, throwing her once-happy family into the depths of despair.
Traditional chemotherapy and radiation therapy once brought a flicker of hope for Mrs. Li, temporarily alleviating her condition. However, fate seemed to play a cruel trick on her again, as the tumor returned with more aggression, no longer responding to conventional treatments. The repeated rounds of therapy took a toll on her body and spirit. Both Mrs. Li and her family were pushed to the brink of collapse, feeling trapped in a deep abyss with no light of hope in sight.
Just when Mrs. Li was about to give up, fate intervened. Thanks to the relentless efforts of the “Advanced Medicine in China” team, they successfully connected Mrs. Li with the country’s top hematology specialists. After a series of communications and coordination, this expert became her last lifeline, taking on the responsibility of devising the best treatment plan during her darkest hours.
After conducting a comprehensive and detailed examination of Mrs. Li, the expert, relying on extensive experience and professional judgment, decisively recommended CAR-T therapy, a cutting-edge treatment. This innovative immunotherapy acts like a magical key, reactivating the patient’s immune system to precisely target and attack cancer cells, offering a new glimmer of life. Faced with this final hope, Mrs. Li carefully considered her options and bravely decided to seize it, determined to fight once more for her life.
The results were truly remarkable. CAR-T therapy produced astonishing effects in Mrs. Li, like a dazzling light in the darkness. After just a few weeks, follow-up tests showed that her tumor had significantly shrunk, and the symptoms that had once plagued her improved dramatically. This was a pivotal moment, allowing Mrs. Li and her family to rediscover hope for the future.
In the months that followed, under close monitoring and consolidation treatment, Mrs. Li’s condition stabilized, as though the ferocious beast of cancer had been tamed. Ultimately, she achieved a miracle—her cancer reached complete remission. For Mrs. Li and her family, this was nothing short of extraordinary, filling their hearts with overwhelming joy and gratitude. They were not only rekindled with the flame of hope for life but also deeply thankful to the “Advanced Medicine in China” team and CAR-T therapy.
As the recommending team, “Advanced Medicine in China” feels honored to have witnessed Mrs. Li’s recovery journey. This is not just a victory for one patient but a successful step forward in the ongoing battle against cancer, inspiring the team to continue seeking rays of hope for more patients. Mrs. Li’s story has become a powerful tale of triumph, spreading rapidly among fellow patients. Her courage and perseverance have set an example for many others bravely fighting blood cancer, encouraging them to press on and never give up.
Through Mrs. Li’s case, CAR-T therapy in China has once again demonstrated its immense potential in the treatment of lymphoma. Like a rising star, it is bringing new hope to blood cancer patients worldwide, illuminating their path toward overcoming the disease. In the future, CAR-T therapy in China will undoubtedly create more miracles, offering patients the dawn of life and a brighter future.
To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of <Advanced Medicine in China> for preliminary evaluation!
WhatsApp: +8613717959070
Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#patientstory #CARTTherapy #CancerSurvivor #Lymphoma #LymphomaTreatment #BloodCancerAwareness#MedicalMiracles #ChinasMedicalAdvances #CancerResearch #PatientStories #HopeAgainstCancer #Immunotherapy #FightCancer #CancerRemission #CourageToFight #BreakthroughInMedicine
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Nature Medicine | New Breakthrough in China’s CAR-T Therapy: Significant Progress in Allogeneic CD5 CAR-T Treatment for Relapsed T-ALL
**Nature Medicine | New Breakthrough in China’s CAR-T Therapy: Significant Progress in Allogeneic CD5 CAR-T Treatment for Relapsed T-ALL**

T-ALL
#CAR-TTherapy #TALL #ALL #Leukemia #RelapsedLeukemia #TCellLeukemia #CD5 #CD7 #CART
Recently, a collaborative research study conducted by multiple Chinese medical and research institutions was published in *Nature Medicine*. This study, titled “Allogeneic CD5-specific CAR-T Therapy for Relapsed/Refractory T-ALL: A Phase 1 Trial,” demonstrated the potential of CD5 CAR-T cells in treating relapsed/refractory acute T-cell lymphoblastic leukemia (R/R T-ALL).
### Innovative Therapy Brings Hope
For a long time, patients with relapsed/refractory T-ALL have lacked effective treatment options and faced a poor prognosis. In recent years, CD7 CAR-T cell therapy has shown some efficacy in these patients, but CD7-negative relapse remains a significant challenge. This study focuses on evaluating the safety, efficacy, and pharmacokinetics of CD5 CAR-T cells, offering new insights for future treatments.
The study included 19 patients, most of whom had previously received CD7 CAR-T therapy. Results showed that this therapy was safe, with no dose-limiting toxicity observed, and adverse events were primarily manageable hematologic toxicity. In terms of efficacy, all patients achieved complete remission within 30 days of treatment. The study also demonstrated, for the first time, the persistence of CD5 CAR-T cells in the body and their ability to eliminate CD5+ T cells, indicating strong anti-tumor activity.
### Breakthrough in Treating Relapsed Patients
In addition to safety and efficacy, the research team explored the coexistence of CD7 CAR-T and CD5 CAR-T cells and studied immune cell changes in the patients. For those who relapsed after CD7 CAR-T treatment with CD7-negative cells, CD5 CAR-T offered a new salvage therapy, providing additional treatment options for such patients.
### Multidisciplinary Collaboration Drives Clinical Progress
Unlike CAR-T therapies for B-cell tumors, treating T-cell malignancies poses more challenges, particularly in controlling immune deficiencies. Dr. Jing Pan and her team conducted in-depth research on target selection and relapse mechanisms, while also focusing on balancing treatment safety and efficacy.
This study was made possible by the collaborative efforts of various medical institutions in China, collectively opening up a new therapeutic pathway for T-cell tumor patients.
### Looking Ahead
As innovations and advances in T-ALL treatment continue, the team plans to further research CD5 CAR-T therapy and collaborate with experts across various fields to optimize CAR-T treatment protocols, helping more patients with T-cell lymphoblastic tumors overcome their diseases.
This series of research achievements not only brings new hope to patients with R/R T-ALL but also provides valuable insights for the future development and optimization of CAR-T therapies. The team remains committed to a patient-centered approach, striving to drive continuous breakthroughs and innovations in T-cell tumor treatment.
To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of <Advanced Medicine in China> for preliminary evaluation!
WhatsApp: +8613717959070
Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#Immunotherapy #CancerTreatment #TALLResearch #LeukemiaBreakthrough #Hematology #CellTherapy #CancerInnovation #CancerResearch #ClinicalTrials #MedicalBreakthrough
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

China’s BCMA CAR-T Therapy Offers Last Hope for Relapsed Multiple Myeloma Patients
### China’s BCMA CAR-T Therapy Offers Last Hope for Relapsed Multiple Myeloma Patients

CAR-T Therapy
Multiple myeloma remains a difficult-to-cure disease, and every year, countless patients around the world face this devastating diagnosis. While treatment options have improved in recent years, and patients’ survival times have extended, drug resistance remains a significant challenge. For patients who have experienced multiple relapses and are resistant to various treatments, the future can seem bleak. Fortunately, with the emergence of **BCMA CAR-T cell therapy**, a new ray of hope is illuminating the path for these patients.
This is the story we’re sharing today, about a 76-year-old female patient who regained control of her life through CAR-T therapy.
#### The First Encounter with the Disease
In 2020, this Chinese 76-year-old woman noticed a decline in appetite and a rapid weight loss, accompanied by persistent rib pain. She had no idea that these symptoms were early signs of multiple myeloma. After several medical tests, her Chinese doctors confirmed the diagnosis: 31% of her bone marrow cells were plasma cells, her M-protein levels reached 85.7 g/L, and calcium levels in her blood were abnormally high. Multiple bones throughout her body also showed signs of significant damage.
The diagnosis left the patient shocked and confused. Multiple myeloma wasn’t her first health challenge; she also had a history of Parkinson’s disease. However, she remained hopeful, believing that with the right treatment, her condition could be controlled. But fate had other plans.
#### The Struggle and Relapse
At the beginning of 2023, the patient’s condition relapsed rapidly. Due to a prolonged lack of regular treatment, her disease worsened, and she became resistant to many standard therapies. After extensive tests, her medical team discovered that she had a high-risk mSMART 3.0 profile, with genetic abnormalities including 1q21 amplification and a t(4;14) translocation, making her prognosis extremely poor. She was now considered a “triple-refractory” patient, resistant to three main treatment categories.
Faced with this complex and challenging situation, the Chinese doctors didn’t give up. After multiple discussions and research, they recommended a cutting-edge therapy — **BCMA CAR-T cell therapy**. This treatment involves modifying the patient’s immune cells to target and destroy cancer cells. However, to undergo this advanced therapy, the patient first needed to undergo **bridging treatment** to reduce the tumor burden in her body.
#### Bridging Treatment: A Turning Point
To prepare for CAR-T therapy, the Chinese doctors initially prescribed the **DKD regimen**, a combination therapy intended to quickly reduce the cancer cell load. However, the first treatment cycle didn’t bring significant improvement, and her free light chain levels remained high. Both the patient and her family felt disappointed, but the Chinese doctors acted quickly, switching to the **KAD regimen**, which included **liposomal doxorubicin** to further enhance the treatment’s effectiveness.
This adjustment brought immediate results. After a few weeks, her free light chain levels began to drop, and her condition showed partial remission (PR). This meant she was finally ready for CAR-T cell therapy.
#### The Miracle of CAR-T Therapy
CAR-T therapy is a breakthrough technology where the patient’s immune cells are extracted, genetically modified to recognize and destroy cancer cells, and then reintroduced into the body. These engineered cells act like precision-guided weapons, specifically targeting her cancer cells.
The patient responded positively to the treatment. Within just a few weeks, her condition was significantly controlled, with results showing a very good partial response (VGPR). For such a complex case of relapsed and refractory disease, this was a major success.
#### The Significance of the Story
This patient’s story highlights China’s latest advancements in the treatment of multiple myeloma. The use of **carfilzomib-based bridging therapy** paved the way for CAR-T therapy, successfully giving a patient with a poor prognosis a new chance at life. For those facing the dual challenges of drug resistance and relapse, **BCMA CAR-T therapy** offers not just a new treatment option, but a lifeline.
The product that has renewed hope for this 76-year-old Chinese woman is a BCMA-targeted CAR-T therapy that has already been launched in China. China is changing the fate of patients worldwide through advanced cancer treatments. Notably, in the field of CAR-T technology related to hematologic tumors and multiple myeloma, two BCMA CAR-T products have been approved in China. Especially commendable is Reindeer Bio’s independently developed fully human BCMA product, FUCASO, which has achieved an astonishing complete remission (CR) rate of 82.4%, the highest among all globally approved products. An increasing number of foreign multiple myeloma patients are now seeking treatment in China to access better therapies at more affordable prices. As China continues to develop cutting-edge medical therapies, aggressive treatments like CAR-T undoubtedly provide new hope for the future of multiple myeloma treatment.
Follow us for more stories of medical innovation and to witness how miracles of life are born in China!
To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of <Advanced Medicine in China> for preliminary evaluation!
WhatsApp: +8613717959070
Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#MultipleMyeloma #CancerTreatment #CAR_TTherapy #BCMACAR_T #CancerSurvivor #Immunotherapy #ChinaMedicalInnovation #CancerResearch #CancerHope #MedicalBreakthrough #MyelomaAwareness #AdvancedCancerCare #RelapsedMyeloma #LifeSavingTreatment #PatientSuccessStory #CancerCare #GlobalHealth #CAR_TSuccess #Oncology #CancerSupport
#ChineseMedical #ChinaHealthcare #MedicalCareInChina #HealthcareInChina · #USMedical #USHealthcare #HealthcareInUSA #AmericanMedical #MedicalCareInUSA #USAHealth #AmericanHealthcare
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Why Does China Have a Unique Advantage in the Field of CAR-T Therapy?
**Why Does China Have a Unique Advantage in the Field of CAR-T Therapy?**

CAR-T
#CAR_Therapy #CancerTreatment #MedicalInnovation #ChinaMedical
In recent years, China has made rapid advancements in medical technology, particularly in the area of CAR-T (Chimeric Antigen Receptor T-cell) therapy. This cutting-edge cancer treatment involves reprogramming a patient’s own T cells to recognize and attack cancer cells. This revolutionary therapy has transformed treatment options for various malignancies, with China’s innovations and applications standing out globally.
### 1. **Scientific Innovation and Technological Breakthroughs**
China has reached a world-leading level in CAR-T research and development. Numerous prestigious medical schools and research institutions in China have actively contributed to this field, leading to the creation of several novel CAR-T treatment methods. Chinese scientists have pioneered significant innovations in CAR-T cell engineering, toxicity control, and target selection. For example, the CD19 CAR-T therapy for hematologic malignancies is widely used in China. Additionally, the fully human BCMA-targeted CAR-T product, Equecabtagene Autoleucel, used for multiple myeloma, has achieved a complete remission (CR) rate of 82.4%. Recently, *Nature* featured China’s breakthrough in using universal CAR-T for autoimmune diseases. New CAR-T therapies targeting solid tumors are also progressing rapidly.
### 2. **Cost-Effectiveness and Extensive Clinical Application**
Compared to some Western countries, CAR-T therapy in China is more affordable, partially due to lower production and R&D costs. A surge of local pharmaceutical and biotech companies has emerged, promoting the domestic production of CAR-T products and reducing reliance on imported drugs. This efficient supply chain management has not only lowered treatment costs but also made the personalized therapy more accessible to patients. While CAR-T therapy in the U.S. can cost $700,000–$800,000, the cost in China is about one-fifth to one-seventh of that.
Moreover, the faster approval process for clinical trials in China enables researchers to quickly bring new therapies to market, allowing patients earlier access to innovative treatments. This efficiency is supported by streamlined regulatory frameworks and healthcare reforms.
### 3. **Government Policy Support and International Collaboration**
The Chinese government has implemented various policies to strongly support biomedical innovation, including the development and application of CAR-T technology. For example, the National Medical Products Administration (NMPA) has accelerated the approval process for CAR-T therapies, simplifying regulatory procedures, and encouraging international cooperation and technology transfer. Many international pharmaceutical giants have partnered with Chinese companies to jointly advance CAR-T therapy research and commercialization. This openness has established China as a key global center for CAR-T treatment.
### 4. **Large Patient Population Driving Research and Application**
As the most populous country, China has a vast cancer patient population, providing abundant clinical cases and research resources for the application and further optimization of CAR-T therapy. This large patient base allows China to conduct large-scale clinical trials in a short time, accelerating the validation of treatment effectiveness and maturity. In China, not only are there local consensus guidelines for CAR-T usage, but each physician applying CAR-T has significant experience in both initial treatments and post-therapy management.
### 5. **Interdisciplinary Collaboration and Development**
China’s advancements in cellular immunotherapy are not solely dependent on progress in medical fields but are also supported by the integration of interdisciplinary technologies such as artificial intelligence, gene editing, and materials science. For instance, AI is increasingly playing a role in optimizing and personalizing CAR-T therapy designs. Gene editing tools like CRISPR are also widely applied in China for designing CAR-T cells, making them more precise and effective.
### Conclusion
China’s unique advantages in CAR-T therapy stem from continuous scientific breakthroughs, lower treatment costs, strong government support, and a vast patient base. As technology advances and international collaborations deepen, China is poised to play an increasingly important role in the global fight against cancer. CAR-T therapy offers new hope to cancer patients, and China’s innovation and strength are helping bring this hope to fruition sooner.
This is not just China’s advantage; it is a blessing for cancer patients worldwide.
🎉🎉To assess whether the condition is suitable for clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
WhatsApp: +8613717959070
Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
#ChimericAntigenReceptor #CancerResearch #Immunotherapy #ChinaMedicalAdvancements #Biotech #GeneTherapy #CellTherapy #HealthcareRevolution #CancerCare #AIinHealthcare #PrecisionMedicine #GlobalHealth
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Nature Headline! China’s CAR-T Therapy Breakthrough Leads the World—A New Hope for Autoimmune Disease Treatment
🌟 **Nature Headline!** China’s CAR-T Therapy Breakthrough Leads the World—A New Hope for Autoimmune Disease Treatment

Autoimmune
