Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

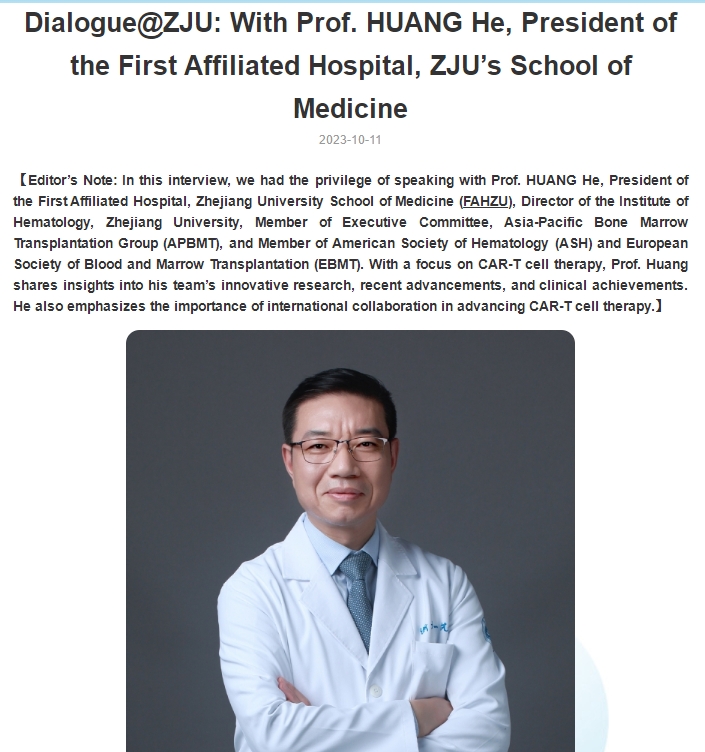
How to Choose Among Similar CAR-T Therapies?
**How to Choose Among Similar CAR-T Therapies?**
Currently, there are multiple CAR-T products targeting the same antigen available on the market, which can make it difficult for patients to decide which one to choose.
Experts recommend selecting a therapy based on the treatment target. It is generally advisable to prioritize approved products, as they have been validated, providing better assurance of safety and efficacy. For example, CD19-targeting CAR-T products are typically preferred over CD22-targeting ones, and BCMA-targeting therapies are favored over GPRC5D-targeting ones.
Additionally, it’s important to consider the origin of the CAR-T cells (such as human-derived vs. mouse-derived) and the costimulatory signals used (e.g., 4-1BB vs. CD28). Different conditions may also influence the choice; for instance, lymphoma patients may be more suitable for CD28, while those with acute leukemia might benefit more from 4-1BB.
In the end, patients are advised to make an informed decision based on their medical history and the guidance of their doctors.

 To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of Advanced Medicine in China for preliminary evaluation!
To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of Advanced Medicine in China for preliminary evaluation!
WhatsApp: Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

At which stage of treatment is the best time to choose CAR-T therapy?
At which stage of treatment is the best time to choose CAR-T therapy?
CAR-T therapy is often used as a last resort, but it should be introduced earlier for better outcomes. Early use, even as a frontline or 1.5-line treatment, could dramatically increase patient cure rates.
Tumor cells are highly adaptable and intelligent, learning to evade treatments over time. Treating tumors early, before they become stronger, is crucial.
CAR-T should not be considered a “last resort” in treatment, as waiting too long may reduce its effectiveness. It’s better to “kill the tumor when it’s young” before it becomes more resilient and difficult to eliminate.

 To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of Advanced Medicine in China for preliminary evaluation!
To assess whether the condition is suitable for CAR-T therapy, you can submit pathology reports, treatment history, and discharge summaries to the Medical Department of Advanced Medicine in China for preliminary evaluation!
WhatsApp: Https://wa.me/+8613717959070
Email: doctor.huang@globecancer.com
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Can the Million-dollar Anti-cancer Injection “Cure” Tumors?
Can the Million-dollar Anti-cancer Injection “Cure” Tumors?
Is CAR-T therapy really a “one-shot cure”?
And how can we ensure that this CAR “drives well and drives long”?
百万抗癌针能“治愈”肿瘤吗?
如何让CAR“开得好,开得久?”
Expert:
**Jing Pan**
**Associate Chief Physician**
**Department of Pediatric Hematology, Beijing Gaobo Hospital**
**Professional Memberships:**
– Member, Pediatric Oncology Professional Committee of the Chinese Anti-Cancer Association
– Youth Committee Member, Hematologic Oncology Professional Committee of the Chinese Anti-Cancer Association
– Youth Committee Member, Clinical Application Professional Committee of the Chinese Medical Biotechnology Association
**Expertise:**
Dr. Pan currently manages an 80-bed pediatric hematology unit and has extensive experience in pediatric hematology, particularly in CAR-T cell immunotherapy, with nearly 10 years of experience in the field. She is dedicated to stratified CAR-T treatment, optimizing the management of complications during CAR-T therapy, and establishing an efficacy monitoring system post-treatment. Dr. Pan and her team have accumulated one of the largest single-center case collections globally, particularly in the areas of sequential CAR-T therapy for improving long-term outcomes in B-ALL and in exploring autologous and allogeneic CD5, CD7 CAR-T therapy for T-ALL/LBL.
Her related clinical research on CD7 CAR-T, CD19 CAR-T, CD22 CAR-T, and CD19-22 sequential CAR-T has been published in leading international journals such as *Lancet Oncology*, *JCO*, *Blood*, *JHO*, and *Leukemia*. Additionally, she has frequently presented the latest advancements in her team’s immunotherapy research at both domestic and international conferences, including ASCO, ASH, EHA, and JSH.
潘 静
副主任医师
北京高博医院 小儿血液科
中国抗癌协会小儿肿瘤专业委员会专业委员
中国抗癌协会血液肿瘤专业委员会青年委员
中国医药生物技术协会医药生物技术临床应用专业委员会青年委员
擅长:
目前独立管理床位数80张的儿童血液病区。从事儿童血液科临床工作多年,特别是在儿童CAR-T细胞免疫治疗方面积累了近10年的经验。致力于CAR-T的分层治疗,优化CAR-T治疗过程中的并发症处理,建立CAR-T治疗后的疗效监控体系。尤其是其带领团队在序贯CAR-T提高B-ALL远期预后,T-ALL/LBL的自体、异体CD5、CD7CAR-T治疗探索方面目前积累了全球较大的单中心病例数。相关的CD7CAR-T临床研究、CD19CAR-T临床研究、CD22CAR-T临床研究、CD19-22序贯CAR-T研究等,发表在国际血液病权威杂志期刊Lancet on-cology、JC0、Blood、JHO和Leukemia。并多次在国内外学术会议(美国临床肿瘤大会ASCO、美国血液年会ASH、欧洲血液年会EHA、日本血液年会JSH)汇报团队免疫治疗的最新进展。

 To assess whether the condition is suitable for clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
To assess whether the condition is suitable for clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
WhatsApp: +8613717959070
Email: doctor.huang@globecancer.com
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79
The Hidden “Anti-Cancer Weapon” in Tumor Tissue – TIL Cells
### The Hidden “Anti-Cancer Weapon” in Tumor Tissue – TIL Cells
TIL Therapy
**TIL Cells: Turning Tumor Tissue “Waste” into Treasure**
**Applications of TIL Cells**
**The Relationship Between TIL Cells and Cancer Patient Prognosis**
**Timing of TIL Cell Storage**
The good news is that several TIL therapies have been officially approved for clinical research in China, targeting various solid tumors such as non-small cell lung cancer, cholangiocarcinoma, esophageal cancer, cervical cancer, ovarian cancer, and breast cancer. Patients seeking to store tumor tissue or seek TIL therapy assistance can consult Advanced Medicine in China
WhatsApp: 137 1795 9070
Email: doctor.huang@globecancer.com
#til #tilcell #cancer #nonsmallcelllungcancer #cholangiocarcinoma #carcinoma #esophagealcancer #cervicalcancer #ovariancancer #breastcancer #tumor #Tiltherapy #ASCO #asco2024 #2024asco
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79
No Tumor Recurrence for Nearly 3 Years, China’s National Research #TIL Therapy #GC101 Targets Various Solid Tumors!
 No Tumor Recurrence for Nearly 3 Years, China’s National Research #TIL Therapy #GC101 Targets Various Solid Tumors!
No Tumor Recurrence for Nearly 3 Years, China’s National Research #TIL Therapy #GC101 Targets Various Solid Tumors!
TIL Therapy
 In recent years, immunotherapy has emerged as a pivotal direction in the future of cancer treatment. Tumor-infiltrating lymphocytes (#TILs) are hailed as the “natural enemies” of cancer cells. TIL therapy developed based on patients’ own tumor-infiltrating lymphocytes boasts advantages such as rich tumor-specific targets, excellent tumor homing capabilities, strong infiltration abilities, and a high safety profile.
In recent years, immunotherapy has emerged as a pivotal direction in the future of cancer treatment. Tumor-infiltrating lymphocytes (#TILs) are hailed as the “natural enemies” of cancer cells. TIL therapy developed based on patients’ own tumor-infiltrating lymphocytes boasts advantages such as rich tumor-specific targets, excellent tumor homing capabilities, strong infiltration abilities, and a high safety profile.
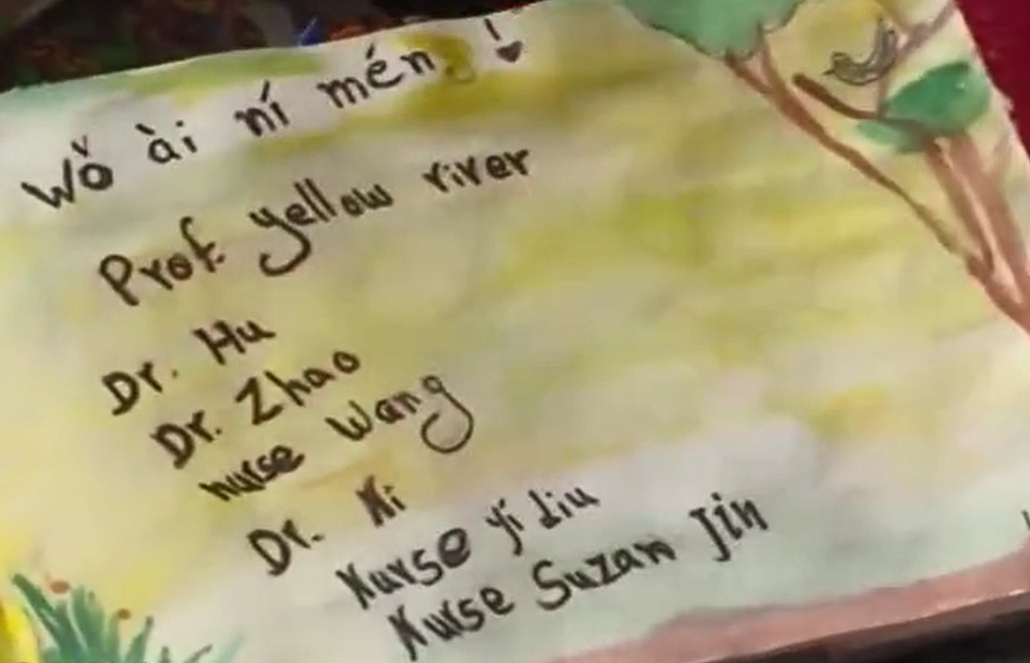
 On February 16, 2024, #Iovance Biotherapeutics announced the #FDA approval of Lifileucel (LN-144) for the treatment of advanced melanoma progressing after PD-1 antibody therapy, marketed as #AMTAGVI™. This marks the global first approval of a TIL therapy and the first approval worldwide for T-cell therapy for solid tumors, marking a significant milestone! #LN144
On February 16, 2024, #Iovance Biotherapeutics announced the #FDA approval of Lifileucel (LN-144) for the treatment of advanced melanoma progressing after PD-1 antibody therapy, marketed as #AMTAGVI™. This marks the global first approval of a TIL therapy and the first approval worldwide for T-cell therapy for solid tumors, marking a significant milestone! #LN144
 On the domestic front in China, several companies have announced good news regarding the clinical approval of TIL pipelines. Overall, the enthusiasm for TIL therapies is on the rise and increasingly intense. Today, let me introduce to you the first independently developed TIL cell therapy #GC101 from Juncell Therapeutics.
On the domestic front in China, several companies have announced good news regarding the clinical approval of TIL pipelines. Overall, the enthusiasm for TIL therapies is on the rise and increasingly intense. Today, let me introduce to you the first independently developed TIL cell therapy #GC101 from Juncell Therapeutics.
 With no tumor recurrence for nearly 3 years, GC01TIL is the first autologous natural tumor-infiltrating lymphocyte injection developed by Juncell Therapeutics, which officially obtained clinical trial implicit approval from the National Medical Products Administration (#NMPA) on April 24, 2022.
With no tumor recurrence for nearly 3 years, GC01TIL is the first autologous natural tumor-infiltrating lymphocyte injection developed by Juncell Therapeutics, which officially obtained clinical trial implicit approval from the National Medical Products Administration (#NMPA) on April 24, 2022.
 Distinguished from Iovance’s approved AMTAGVI™ (#Lifileucel), innovative GC101TIL therapy requires patients to be treated in ordinary wards without the need for high-intensity pre-conditioning before TIL cell infusion or any IL-2 dosage post-infusion. This simplified clinical protocol ensures effective TIL cell proliferation within patients, greatly avoiding the risks associated with AMTAGVI™’s black box warnings (such as treatment-related deaths, persistent severe cytopenia, severe infections, cardiopulmonary and renal function damage), substantially improving the safety, convenience, and accessibility of TIL therapy.
Distinguished from Iovance’s approved AMTAGVI™ (#Lifileucel), innovative GC101TIL therapy requires patients to be treated in ordinary wards without the need for high-intensity pre-conditioning before TIL cell infusion or any IL-2 dosage post-infusion. This simplified clinical protocol ensures effective TIL cell proliferation within patients, greatly avoiding the risks associated with AMTAGVI™’s black box warnings (such as treatment-related deaths, persistent severe cytopenia, severe infections, cardiopulmonary and renal function damage), substantially improving the safety, convenience, and accessibility of TIL therapy.
 Currently, according to the latest revelations from Juncell Therapeutics, the Phase I clinical trial of Juncell Therapeutics’ autologous natural TIL cell injection GC101 is underway in eight authoritative tertiary hospitals in China, achieving significant efficacy.
Currently, according to the latest revelations from Juncell Therapeutics, the Phase I clinical trial of Juncell Therapeutics’ autologous natural TIL cell injection GC101 is underway in eight authoritative tertiary hospitals in China, achieving significant efficacy.
 GC101, targeting various types of advanced solid tumors including malignant melanoma, cervical cancer, and lung cancer, has demonstrated an objective response rate of over 35%. Four patients have achieved complete tumor remission (#CR), with the longest no-recurrence survival period approaching 3 years, without experiencing any severe adverse reactions related to treatment, significantly improving the safety, applicability, and accessibility of #TILtherapy. Let us look forward to more surprises that GC101 will bring in the future!
GC101, targeting various types of advanced solid tumors including malignant melanoma, cervical cancer, and lung cancer, has demonstrated an objective response rate of over 35%. Four patients have achieved complete tumor remission (#CR), with the longest no-recurrence survival period approaching 3 years, without experiencing any severe adverse reactions related to treatment, significantly improving the safety, applicability, and accessibility of #TILtherapy. Let us look forward to more surprises that GC101 will bring in the future!
 Currently, #Juncell Therapeutics’ GC101 clinical trial for the treatment of advanced solid tumors is actively recruiting :
Currently, #Juncell Therapeutics’ GC101 clinical trial for the treatment of advanced solid tumors is actively recruiting :
FOR FREE
 Key Inclusion Criteria:
Key Inclusion Criteria:
1. Aged 18-75 years, regardless of gender;
2. Definitive diagnosis of malignant solid tumors (including but not limited to #melanoma, #lungcancer, #cervicalcancer, #esophagealsquamouscellcarcinoma, #headandnecksquamouscellcarcinoma, #endometrialcancer);
3. Standard treatment failure or lack of effective treatment options;
4. At least 2 lesions, with the physical condition supporting minimally invasive surgical sampling.
 This clinical trial is free of charge for participants. If you wish to participate in this clinical trial, you need to submit your treatment history, recent imaging and blood test reports, infectious disease reports, and discharge summaries to <@Advanced Medicine in China for preliminary assessment.
This clinical trial is free of charge for participants. If you wish to participate in this clinical trial, you need to submit your treatment history, recent imaging and blood test reports, infectious disease reports, and discharge summaries to <@Advanced Medicine in China for preliminary assessment.
 Email: doctor.huang@globecancer.com,
Email: doctor.huang@globecancer.com,
 WhatsApp: +8613717959070
WhatsApp: +8613717959070
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

🎉💉 Exciting Breakthrough Alert! Chinese Medical Team Unveils Game-Changing mRNA Cancer Vaccine 🎉💉
🎉💉 Exciting Breakthrough Alert! Chinese Medical Team Unveils Game-Changing mRNA Cancer Vaccine 🎉💉

Advanced Science
Say hello to the future of cancer treatment! A groundbreaking mRNA cancer vaccine jointly developed by Chinese scientists has hit the spotlight, promising to elevate tumor suppression rates and extend survival periods.
🔬 What’s the Buzz? 🔬
Published in the prestigious journal “Advanced Science”, the research titled “All-Trans-Retinoic Acid-Adjuvanted mRNA Vaccine Induces Mucosal Anti-Tumor Immune Responses for Treating Colorectal Cancer” reveals a novel mRNA cancer vaccine. This vaccine, packaged with lipid nanoparticles (LNPs), delivers All-Trans-Retinoic Acid (ATRA) and mRNA, effectively stimulating mucosal immune responses in the intestines. Compared to conventional mRNA-LNP vaccines, this innovative approach significantly boosts tumor suppression and prolongs survival rates.
🩺 Why It Matters 🩺
Colorectal cancer ranks third in cancer incidence and second in mortality globally. Conventional treatments such as surgery, chemotherapy, and radiation often come with high recurrence rates. Enter cancer immunotherapy—the beacon of hope in the fight against colorectal cancer. Cancer vaccines, a vital component of immunotherapy, harness the body’s immune system to target and destroy cancer cells. With the recent success of mRNA vaccines for COVID-19, mRNA cancer vaccines have garnered immense attention for their potential to revolutionize cancer treatment.
🚀 The Breakthrough 🚀
The key lies in ATRA-LNP’s ability to induce cytotoxic T cells in the intestines, offering a promising therapeutic approach for colorectal cancer. In animal models, ATRA-LNP treatment led to a remarkable reduction in tumor growth and extended survival rates compared to conventional treatments. These findings underscore the potential of mRNA cancer vaccines, particularly in enhancing the treatment outcomes for colorectal cancer patients.
🌟 The Takeaway 🌟
With its ability to activate anti-tumor immune responses at mucosal surfaces, the novel mRNA cancer vaccine brings hope for improved outcomes in colorectal cancer treatment. ATRA incorporation into LNPs not only enhances mRNA delivery efficiency but also directs activated T cells towards the intestines, amplifying their anti-tumor effects. This study paves the way for a promising future in enhancing the efficacy of mRNA cancer vaccines against colorectal cancer.
🎉🎉To assess whether the condition is suitable for CAR-T or clinic therapy, you can submit Advanced Medicine in China for preliminary evaluation!
Email: doctor.huang@globecancer.com,
WhatsApp: 137 1795 9070
#CancerResearch #MedicalBreakthrough #ImmunotherapyInAction #ColorectalCancerFighters #mRNA #CancerVaccine #vaccine #colorectal #colorectalcancer #cancerfighters #chinesemedical #cancertreatment #tumor
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Breakthrough! Chinese Novel CAR-T Therapy Kills Tumors and Prevents Relapse!
🌟✨ **Breakthrough! Chinese Novel CAR-T Therapy Kills Tumors and Prevents Relapse!** ✨🌟

CAR-T Therapy
🔬 On January 2, 2024, a groundbreaking clinical study from China was published in *Nature*. This study, employing engineering design, enables CAR-T cells to secrete Interleukin-10 (IL-10), thereby enhancing metabolism within the tumor microenvironment. The modified IL-10 CAR-T cells increase oxidative phosphorylation in a mitochondrial acetoacetate carrier-dependent manner, resulting in complete regression of solid tumors and metastatic cancers, including colon cancer, breast cancer, melanoma, and pancreatic cancer. This breakthrough research offers new hope for cancer patients.
🌱 **The Miracle of IL-10** 🌱
The secretion of IL-10 promotes the proliferation and effector functions of CAR T cells, leading not only to the regression of solid tumors but also inducing stem cell-like memory responses in lymphoid organs, providing enduring protection against tumor re-attack. Specifically, IL-10 HER2 CAR-T cells achieved complete regression of MC38-HER2 tumors in mice, with a cure rate of 90%. In the case of melanoma, IL-10 TRP-1 CAR-T cells achieved a clearance rate of 60%, with significant success in treating the orthotopic B16F10 melanoma model.
🦠 **A Weapon against Relapse** 🦠
In addition to complete regression of solid tumors, IL-10 CAR-T cells demonstrated the ability to prevent relapse in immunodeficient mice. Mice treated with IL-10 CD19 hCAR-T cells for Raji or PANC1-CD19 tumors exhibited complete tumor regression without relapse, indicating stronger anti-tumor capabilities of IL-10 CAR-T cells in xenograft models. Particularly noteworthy is the effective elimination of pancreatic ductal adenocarcinoma (PDAC) tumors by IL-10 CD19 hCAR-T cells, resulting in complete response in all treated mice.
💊 **A Revolutionary Treatment Approach** 💊
These findings suggest that IL-10-expressing CAR-T cells are an effective immunotherapy against various solid tumors, capable of achieving complete regression in multiple synthetic and xenograft tumor models. What’s more exciting is that preliminary results indicate the metabolism-enhanced IL-10 CD19 CAR-T cell therapy developed by Leman Biotech requires extremely low treatment doses, consistently achieving complete remission in numerous relapsed/refractory lymphoma or leukemia patients, paving the way for a new era in cancer treatment.
✨ **A Beacon of Hope** ✨
This breakthrough study brings hope to cancer patients and demonstrates the immense potential of CAR-T therapy in cancer treatment. Looking ahead, further advancements in this technology promise to provide more opportunities for recovery and survival to patients worldwide. Let’s anticipate more breakthroughs together and strive towards conquering cancer
#all #CARTtherapy #CancerTreatment #RRMM #IL10 #Tumor #Nature #MedicalBreakthrough #CARTCELL #coloncancer #breastcancer #melanoma #pancreatic 🌟🔬💊
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Revolutionizing Medicine: CAR-T Therapy Beyond Cancer
🚀Revolutionizing Medicine: CAR-T Therapy Beyond Cancer 🚀

🔬 Over the past decade, CAR-T cell therapy has transformed the field of oncology, successfully treating previously incurable blood cancers. While CAR-T therapy gained fame for its success in cancer treatment, the roots of this groundbreaking principle trace back nearly 30 years—initially exploring T cell therapy for HIV/AIDS. Although the early attempts didn’t succeed in treating HIV/AIDS, they demonstrated the enduring potential of engineered T cells in immunocompromised patients.
🚀 The future of CAR-T therapy holds vast potential in reshaping the landscape of medical treatment, reaching far beyond the realms of cancer. Stay tuned for ground
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

A Miraculous Journey: Israeli Artist Finds Cure for Multiple Myeloma in Hangzhou China


Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79

Clinical Breakthrough: Chinese CAR-T – Inaticabtagene Autoleucel Revolutionizing Hematologic Cancer Therapy

Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79
Breakthrough Advances in CAR-T Cell Therapy Combined with TKI for Malignant Hematologic System Tumors

Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 78
Warning: Trying to access array offset on value of type bool in /www/wwwroot/www.medtourcn.com/wp-content/themes/medical-directory/framework/theme/medicaldirectory-image.php on line 79
A significant breakthrough in Chinese solid tumor CAR-T therapy, resulting in complete remission for pancreatic cancer patients.